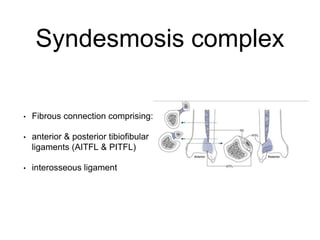
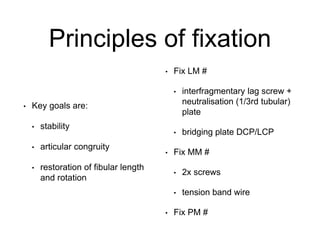
This document discusses surgical techniques for fixing ankle fractures. It describes the anatomy of the ankle joint and surrounding ligaments. Common fracture patterns are described using the Weber classification system. Surgical approaches and fixation methods are outlined, including lateral plating, lag screws, and posterior plating. The principles of fixation aim for stability, articular congruity, and restoration of the fibula. Factors such as the position of the foot, deforming forces, and stability tests are important to consider when determining appropriate treatment.