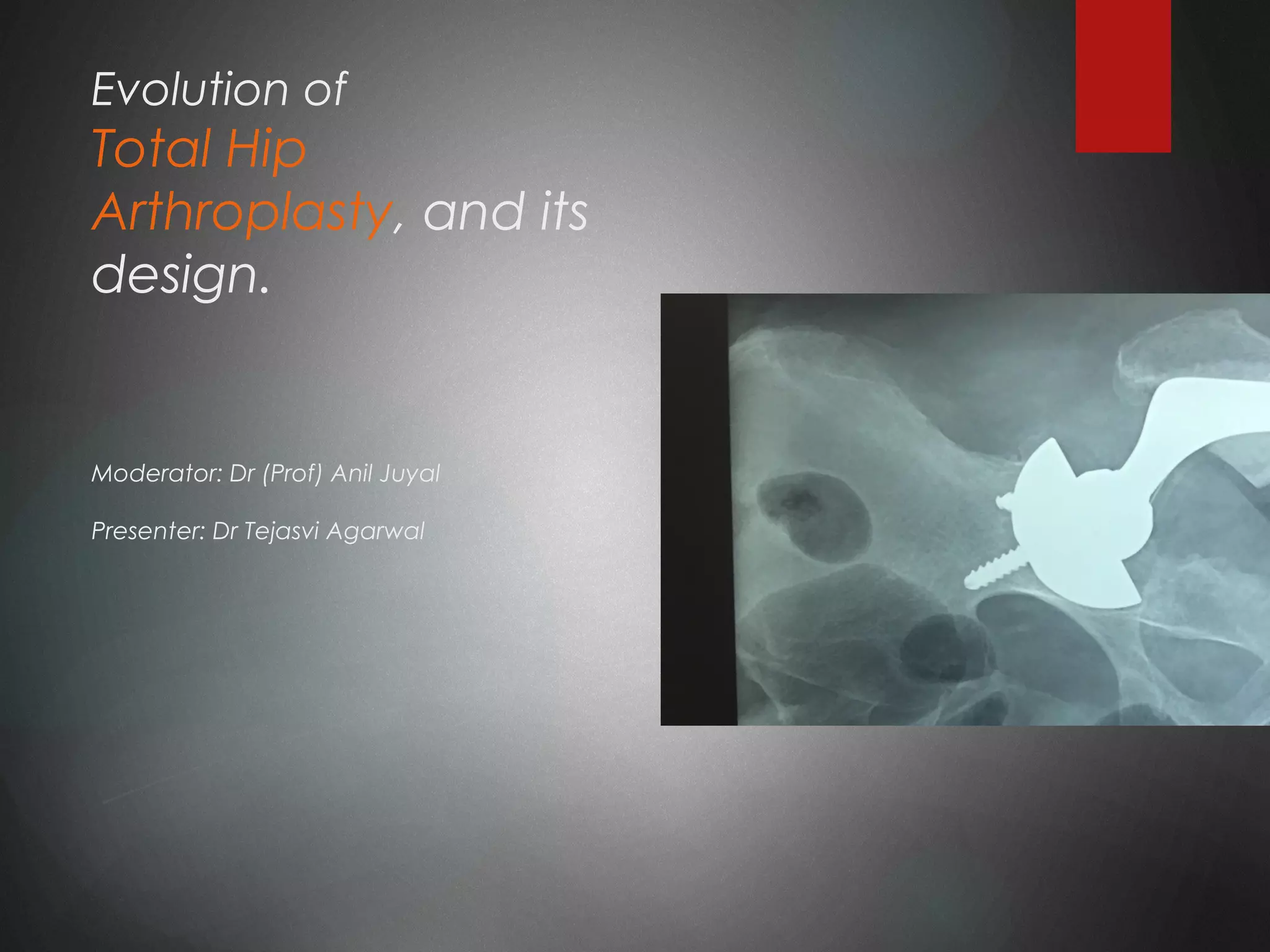
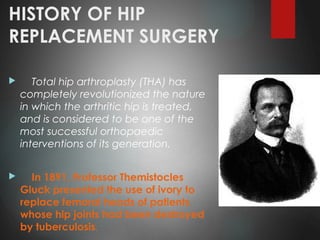
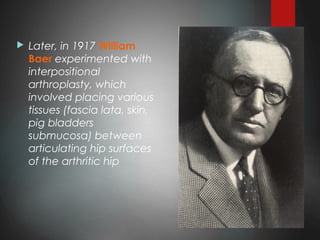
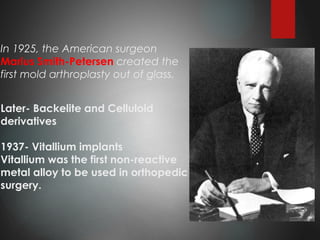
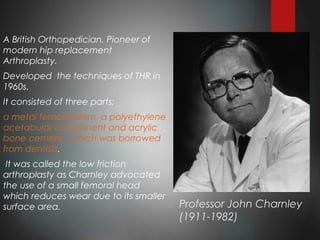
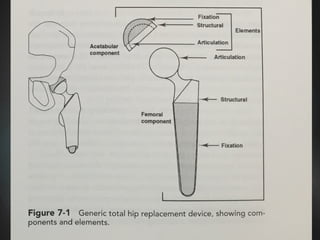
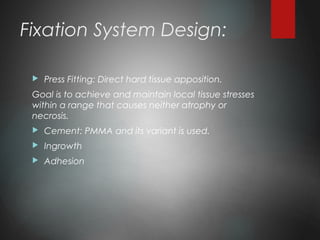
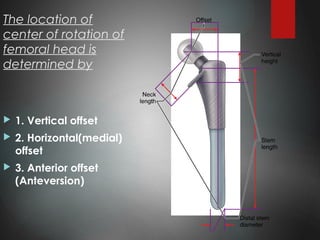
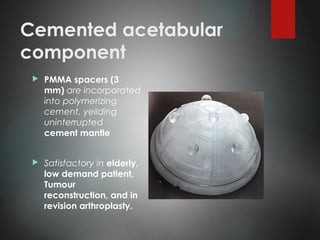
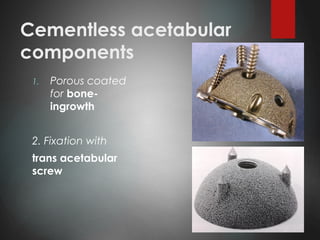
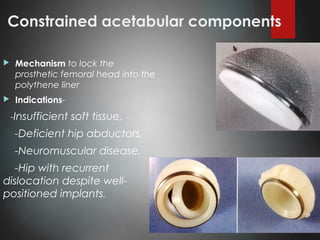
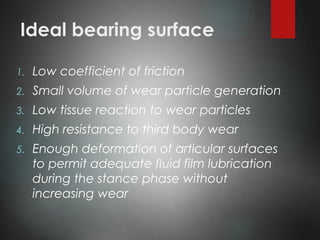
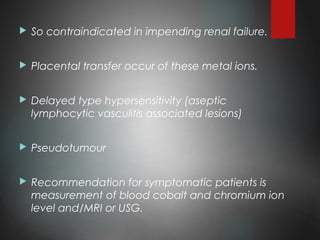
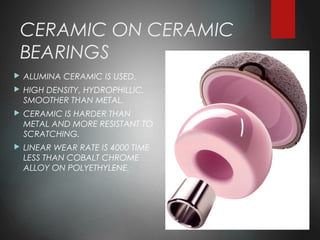
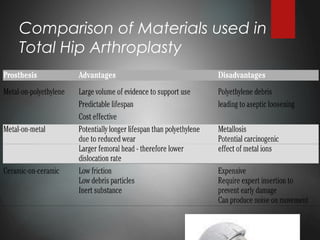
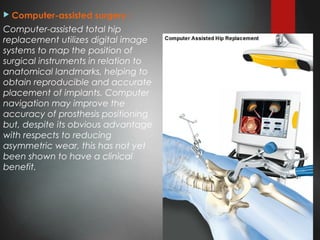
This document discusses the history and evolution of total hip arthroplasty (THA) and hip replacement component designs. It outlines key developments from the late 19th century experiments with ivory and tissue replacements, to modern THA pioneered by Professor Charnley in the 1960s using bone cement and low friction materials. Current designs aim to restore normal hip biomechanics and include cemented or cementless femoral and acetabular components with various fixation methods and bearing surfaces to reduce wear. Future advances focus on minimally invasive techniques, computer navigation, and developing more durable and compliant bearing materials to improve implant longevity.