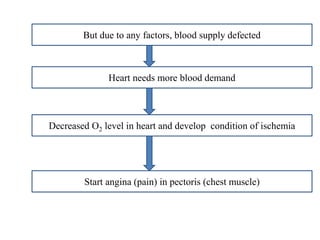
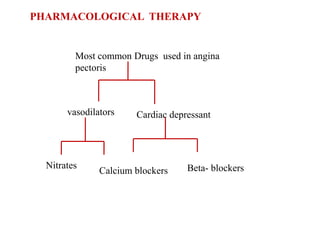
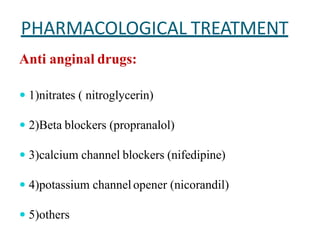
The document provides a comprehensive overview of angina pectoris, including its definition, types (stable, unstable, variant), and epidemiology, affecting approximately 112 million people globally. It discusses various risk factors, both modifiable and non-modifiable, as well as the etiology, pathophysiology, clinical manifestations, and diagnostic measures for angina. Management strategies are also detailed, covering non-pharmacological approaches and pharmacological treatments, including the use of nitrates and beta-blockers.