This document describes the components and functioning of an anesthesia machine. It discusses:
- The history of anesthesia machines and their development over time.
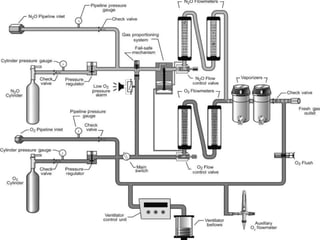
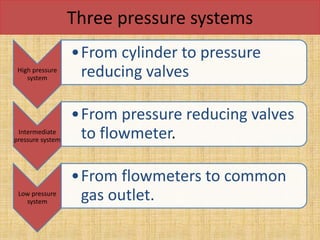
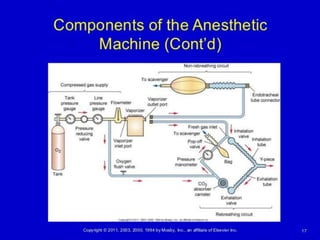
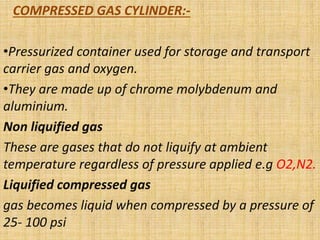
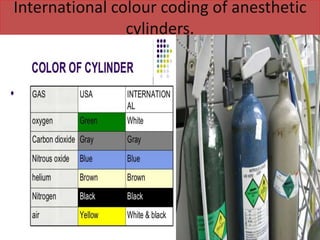
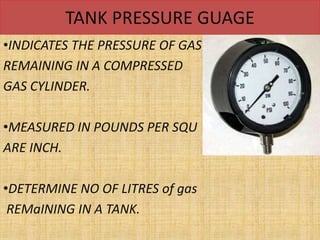
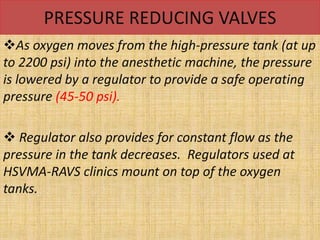
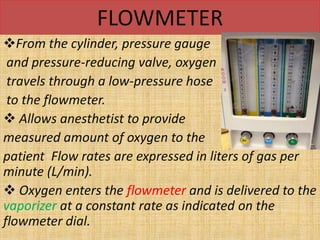
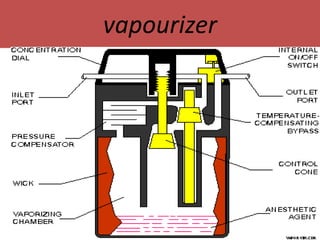
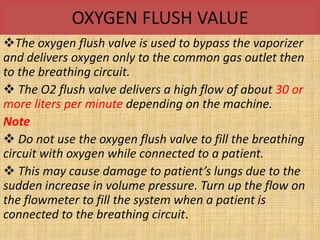
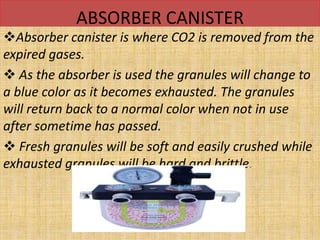
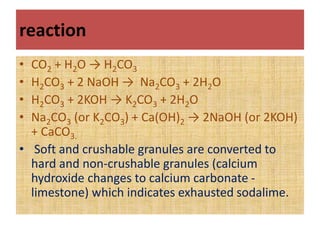
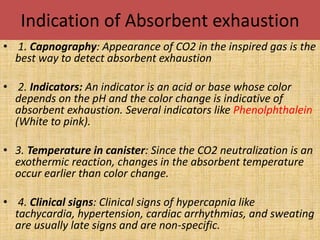
- The main components including gas cylinders, pressure regulators, flowmeters, vaporizers, breathing systems, and absorber canisters.
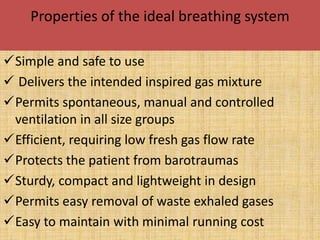
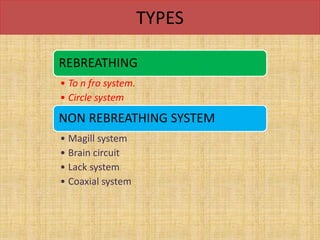
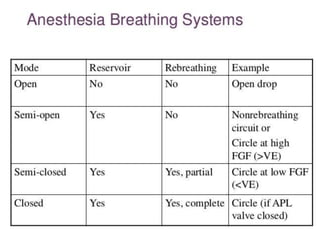
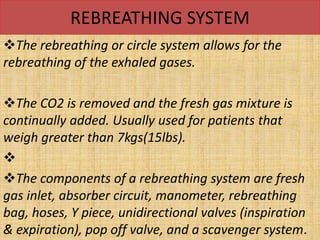
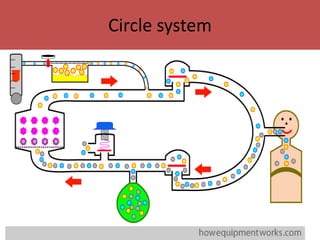
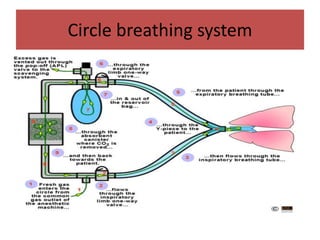
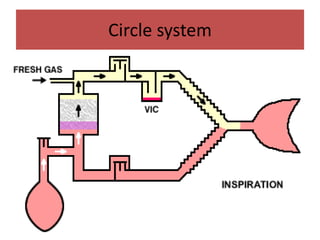
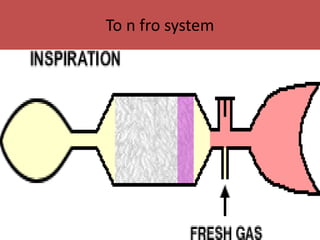
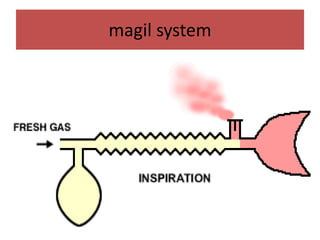
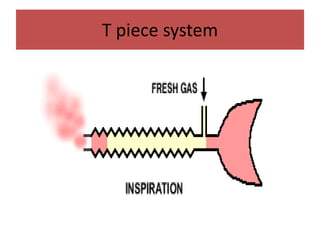
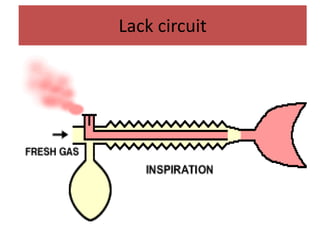
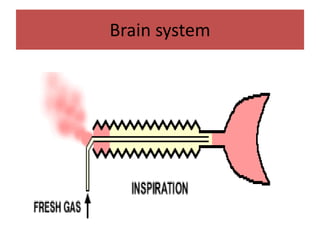
- The differences between rebreathing and non-rebreathing breathing circuits. Rebreathing circuits allow for reuse of exhaled gases while non-rebreathing circuits do not.
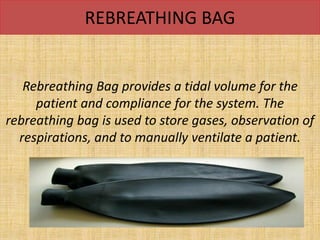
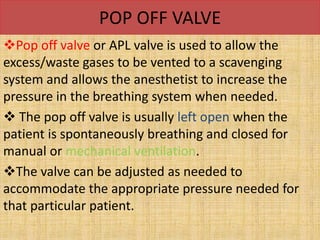
- Key parts like the fresh gas inlet, unidirectional valves, rebreathing bag, and pop-off valve that control gas flow within the breathing system.