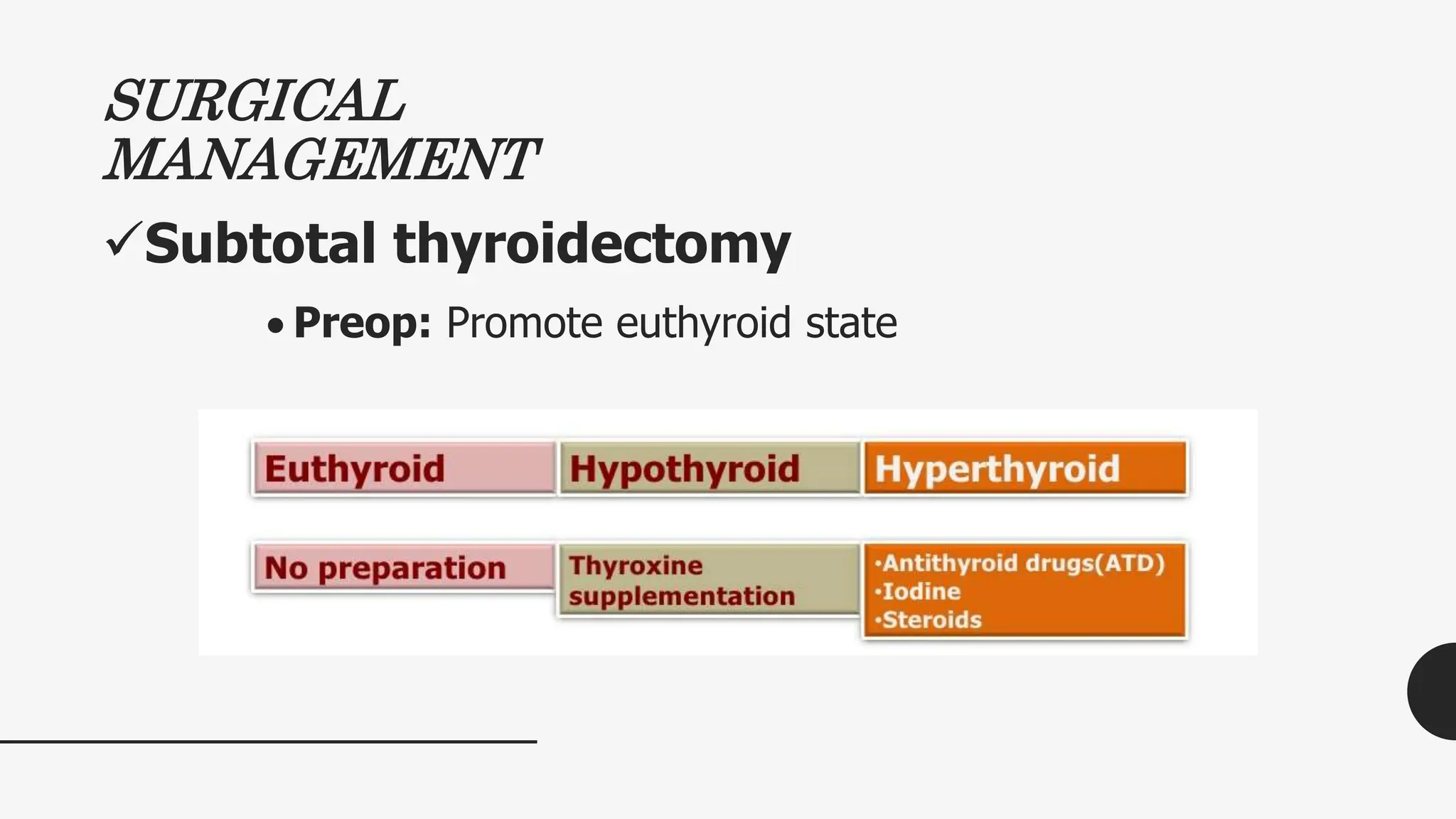
The document discusses thyroid and parathyroid disorders, outlining conditions such as goiter, hypothyroidism, and hyperthyroidism, along with their causes, clinical manifestations, nursing diagnoses, and management strategies. It emphasizes the importance of restoring normal metabolic states, managing symptoms, and educating patients about lifelong therapies and dietary considerations. Additionally, it addresses the roles of medications, interventions, and evaluations in the treatment and monitoring of these endocrine disorders.









































































![Intervention (Hypercalcemic Crisis)
Rehydration with IV fluids
Diuretics
Phosphate therapy
Biphosphonates (eg, etidronate [Didronel]) – prevent loss of
bone density
Pamidronate [Aredia]) – to treat high blood calcium levels;
diseases that causes abnormal & weak bones
Cytotoxic agents ( Mithramycin), calcitonin (to decrease
skeletal Ca release and increase renal clearance of Ca),
and dialysis](https://image.slidesharecdn.com/4-240525034446-2eccea34/75/THYROID-PARATHYROID-medical-surgical-nursing-77-2048.jpg)

