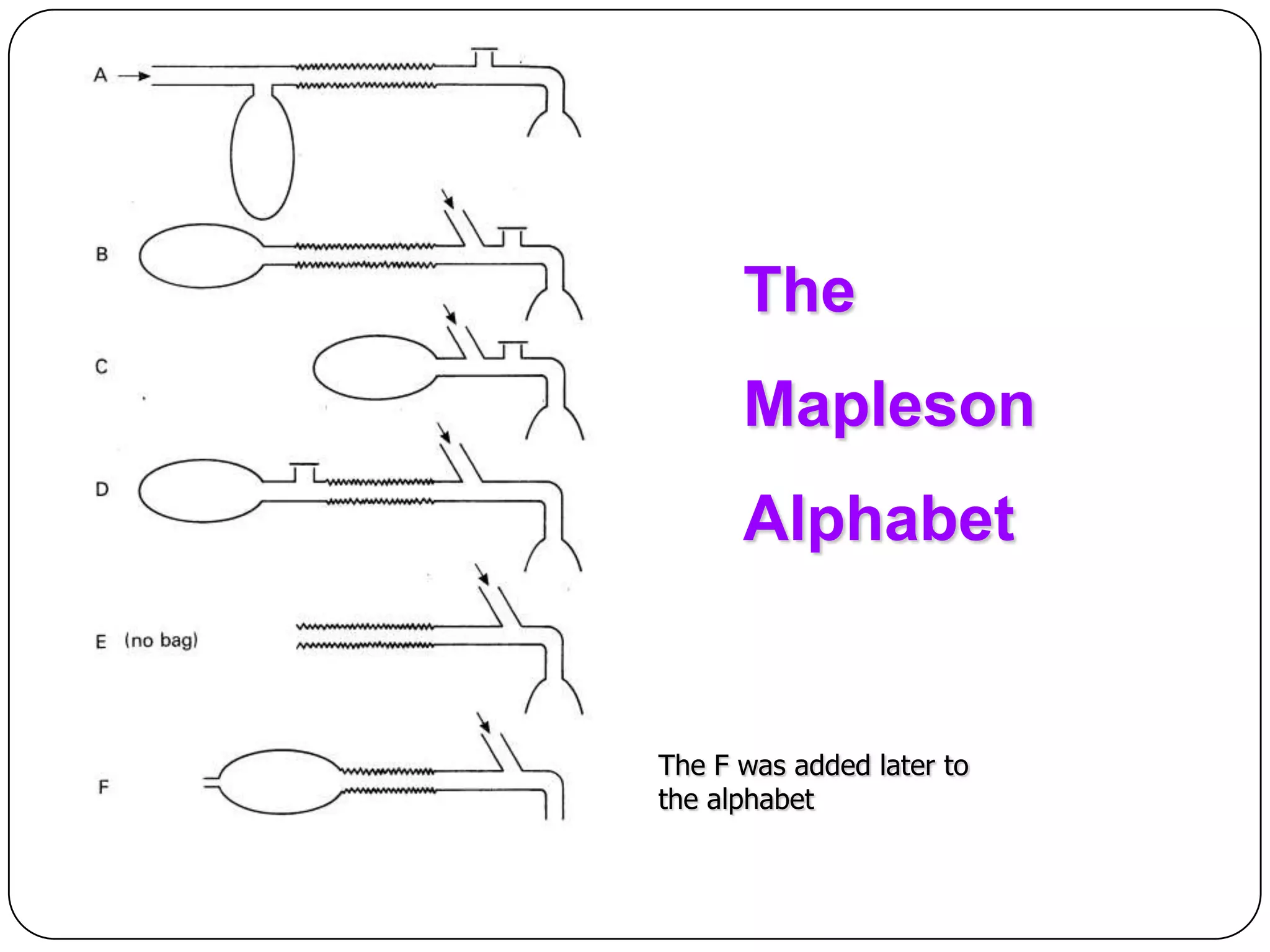
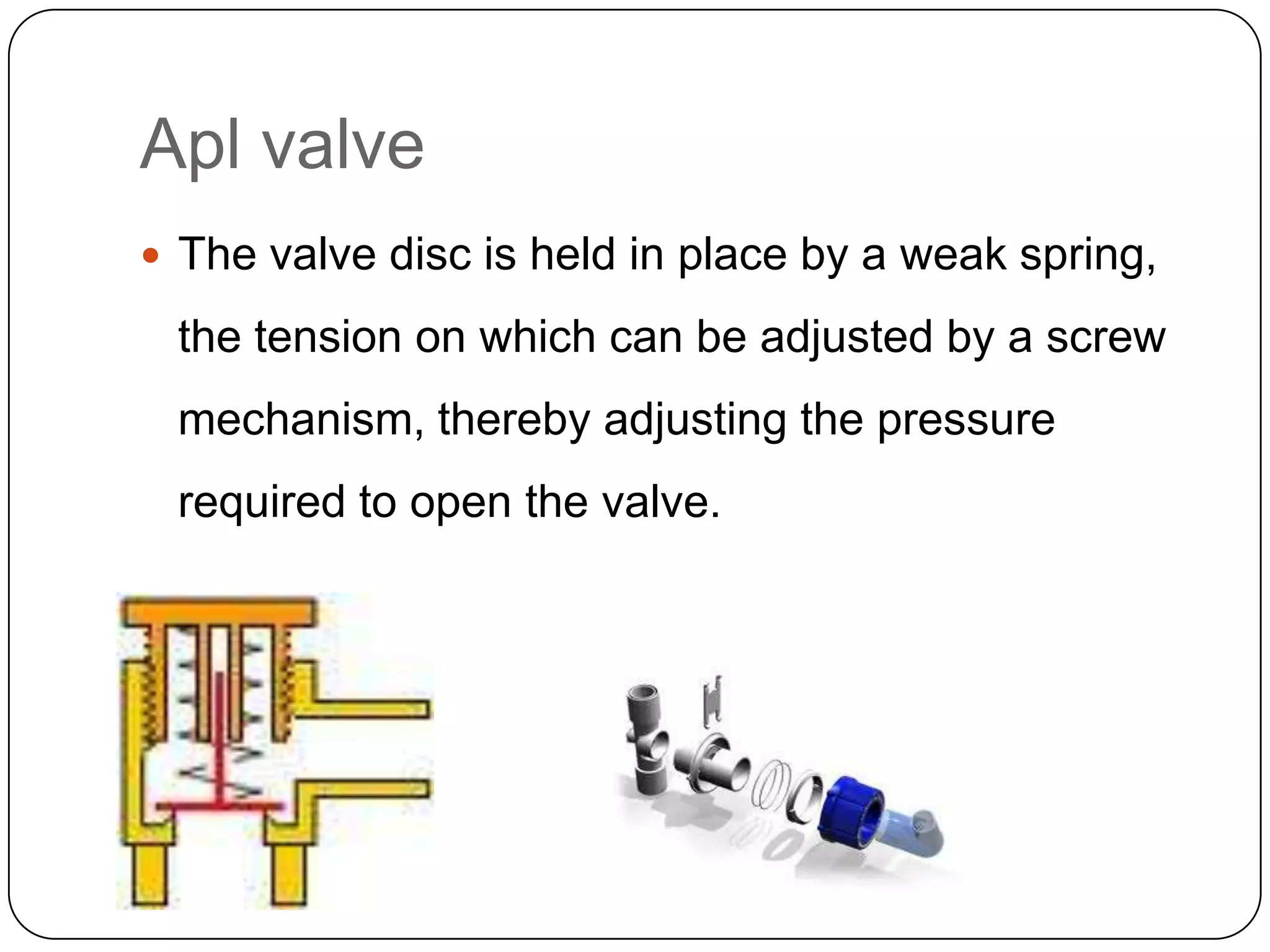
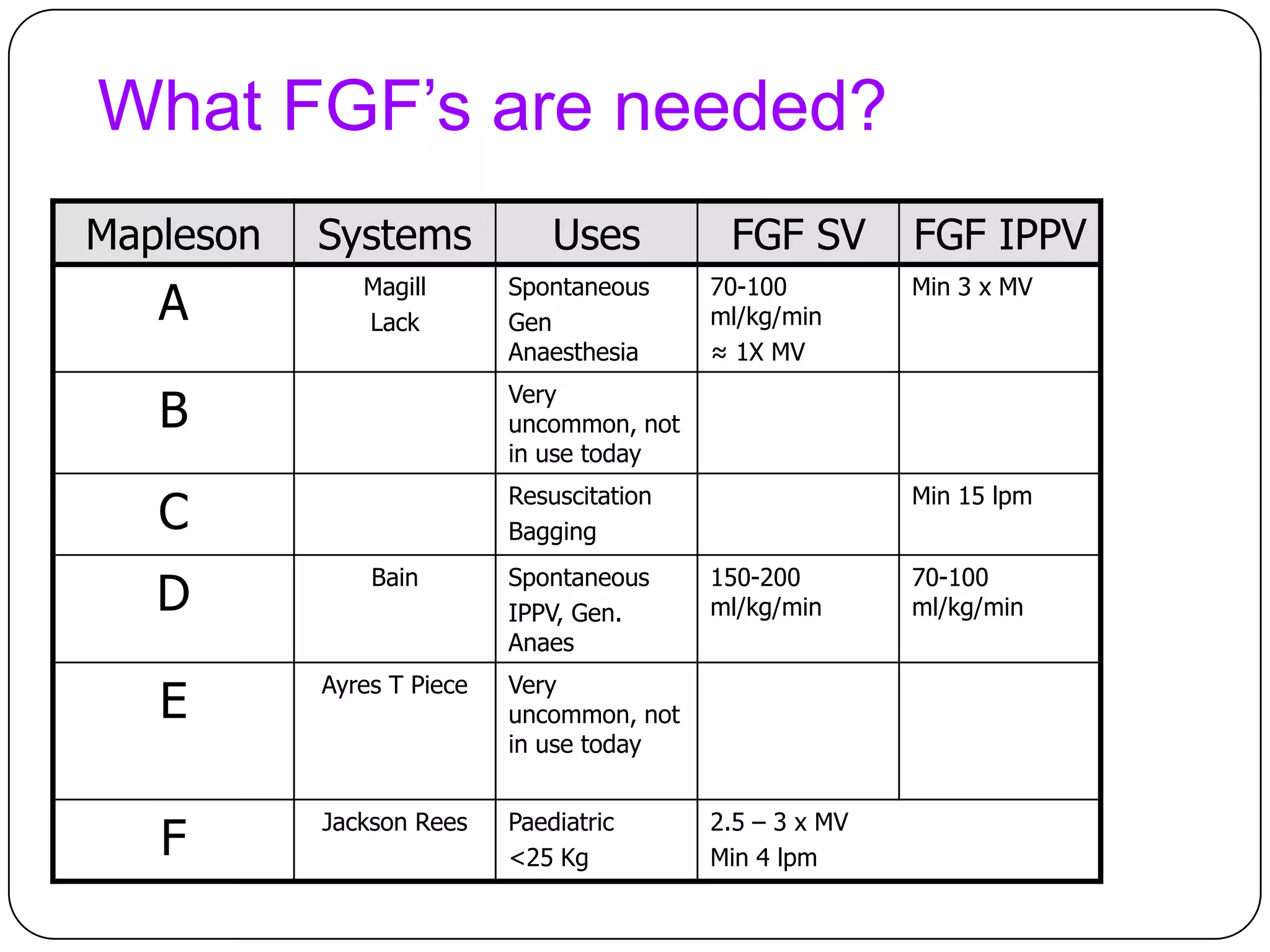
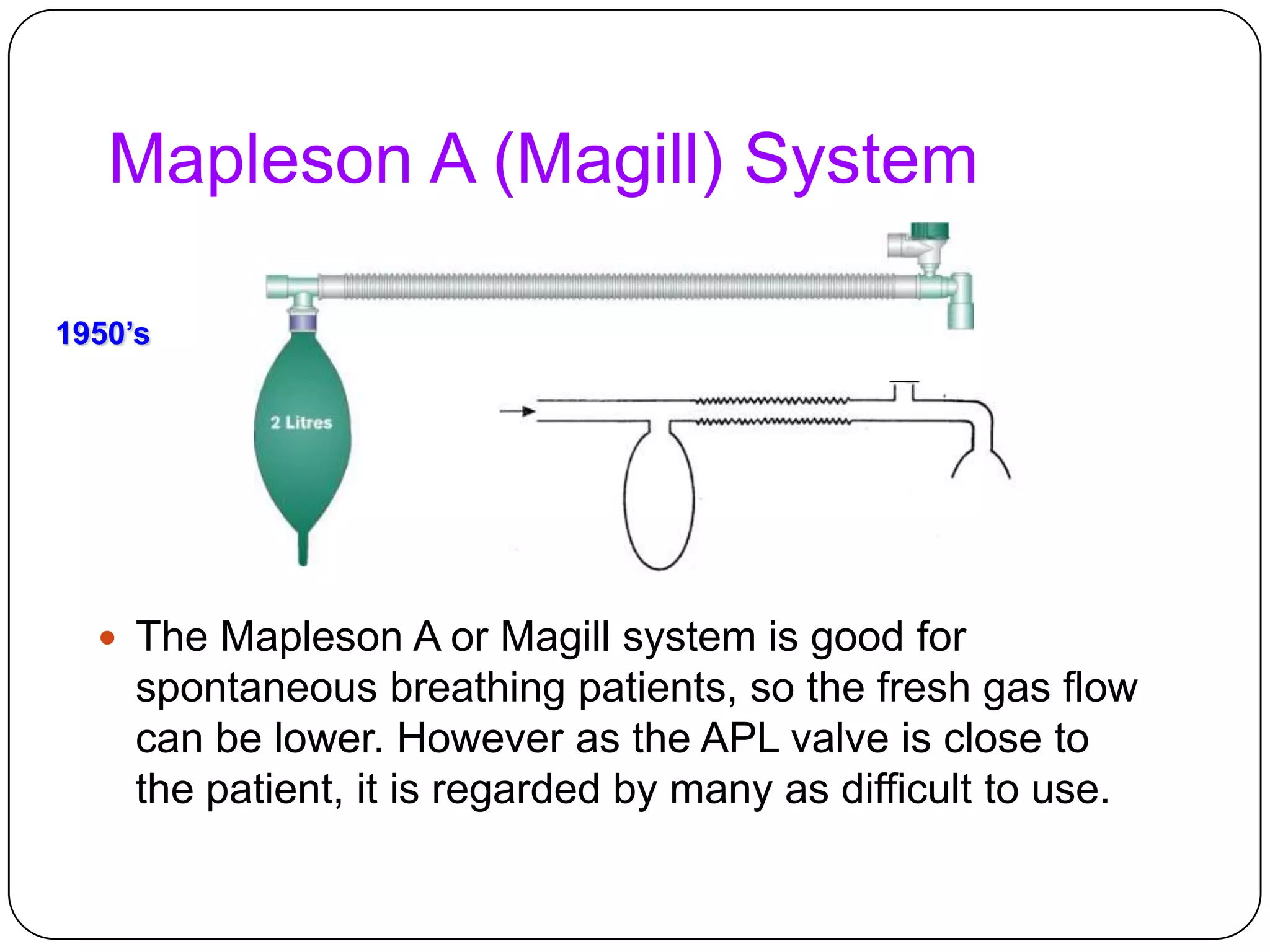
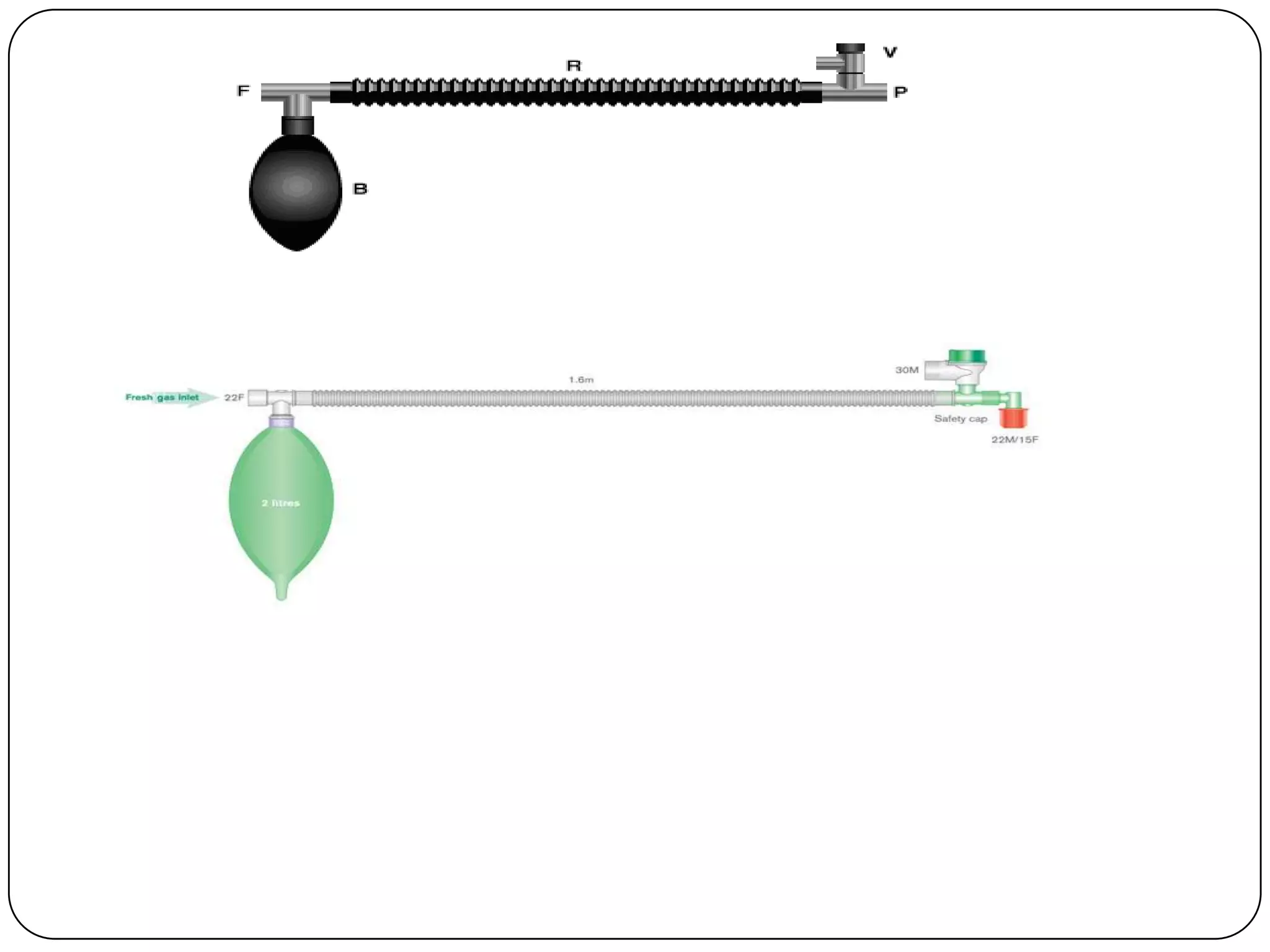
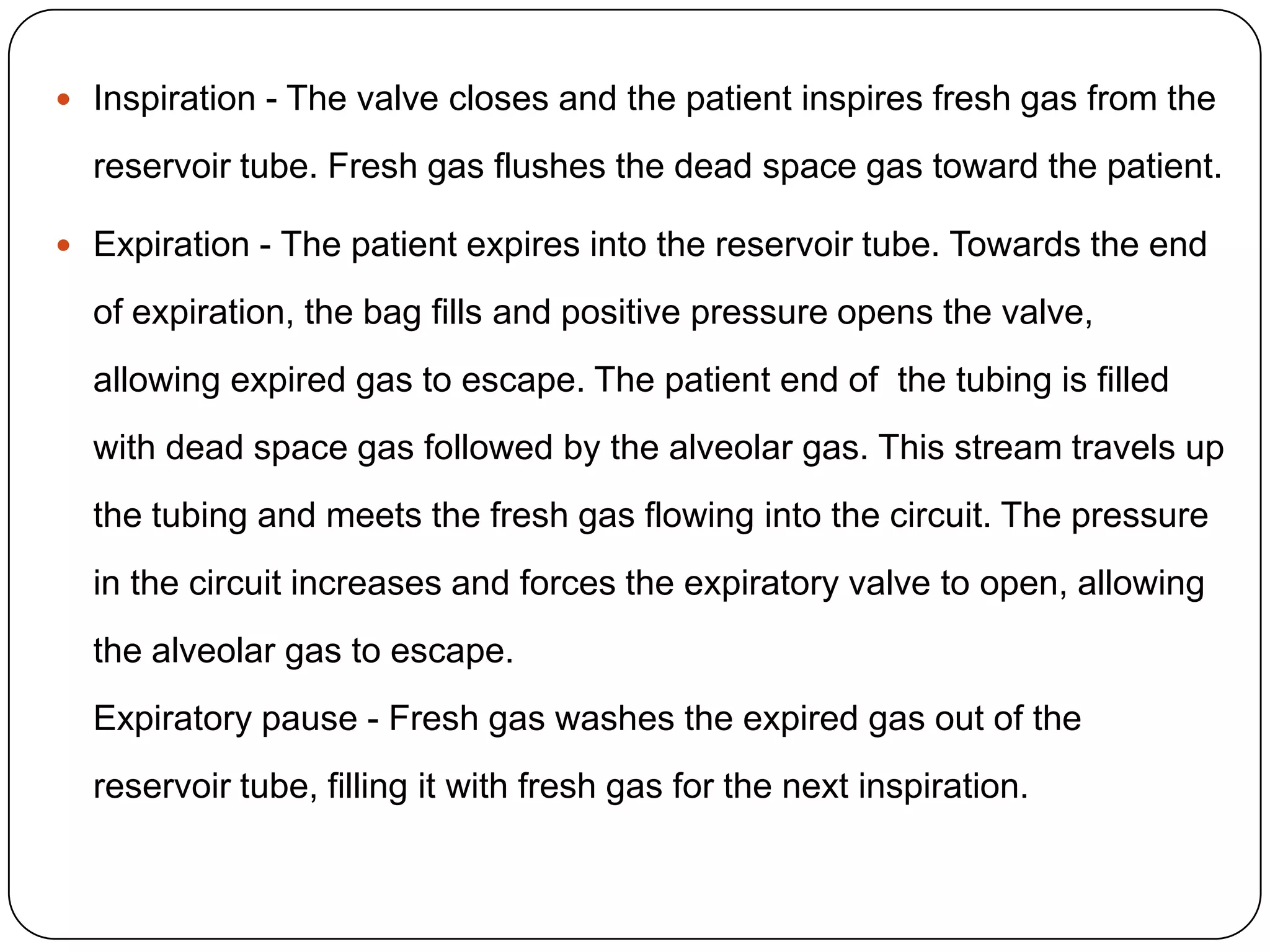
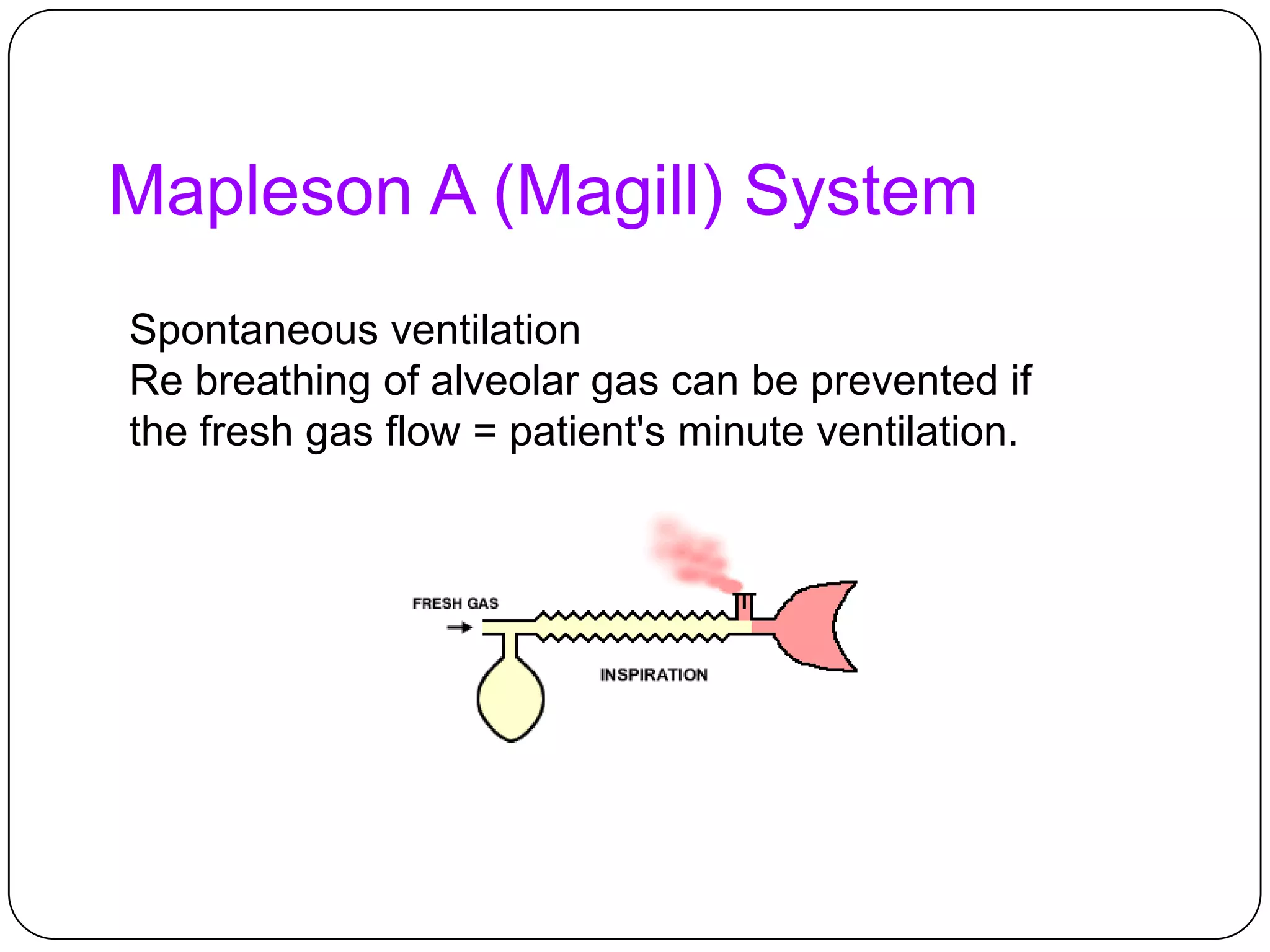
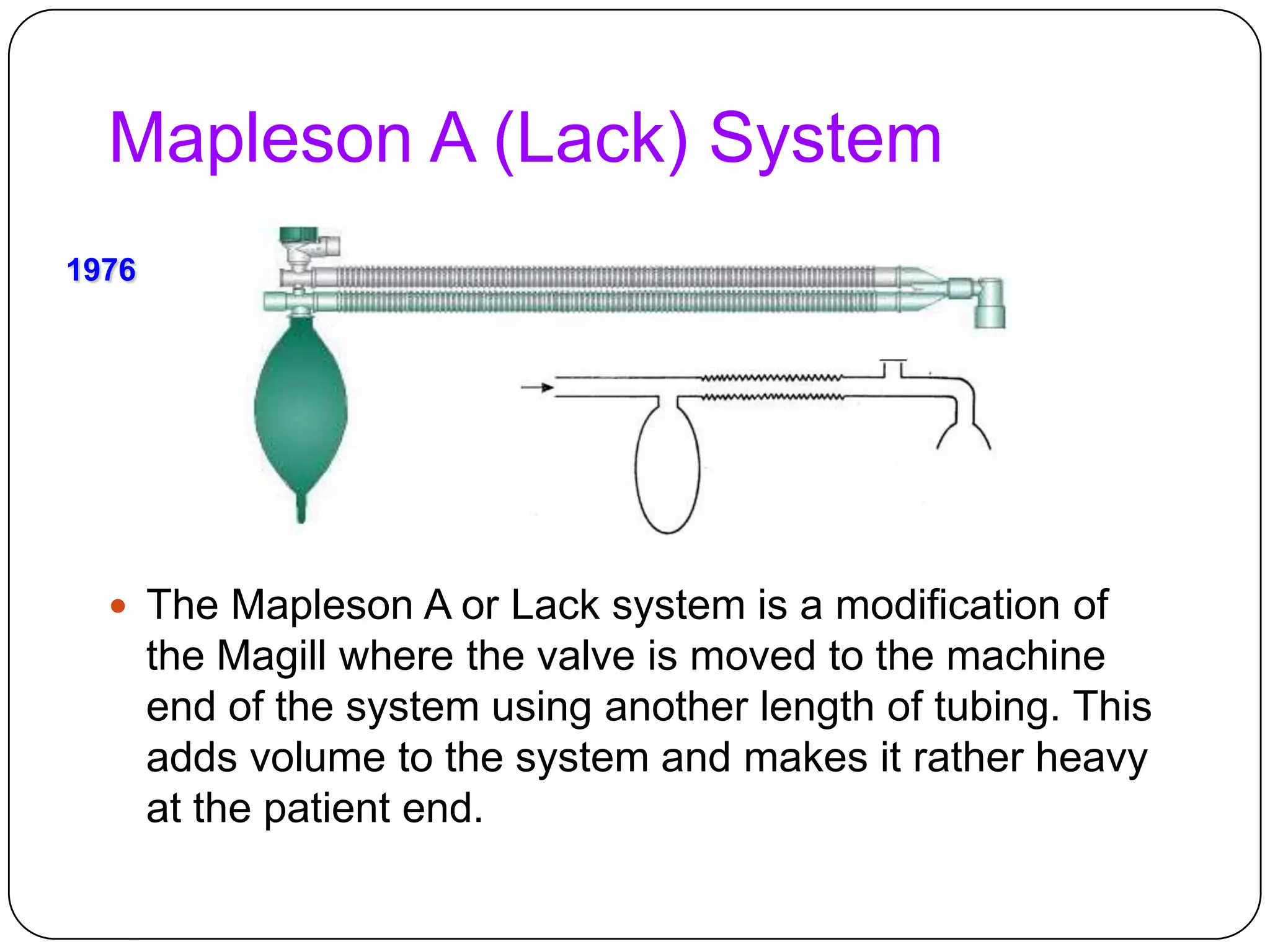
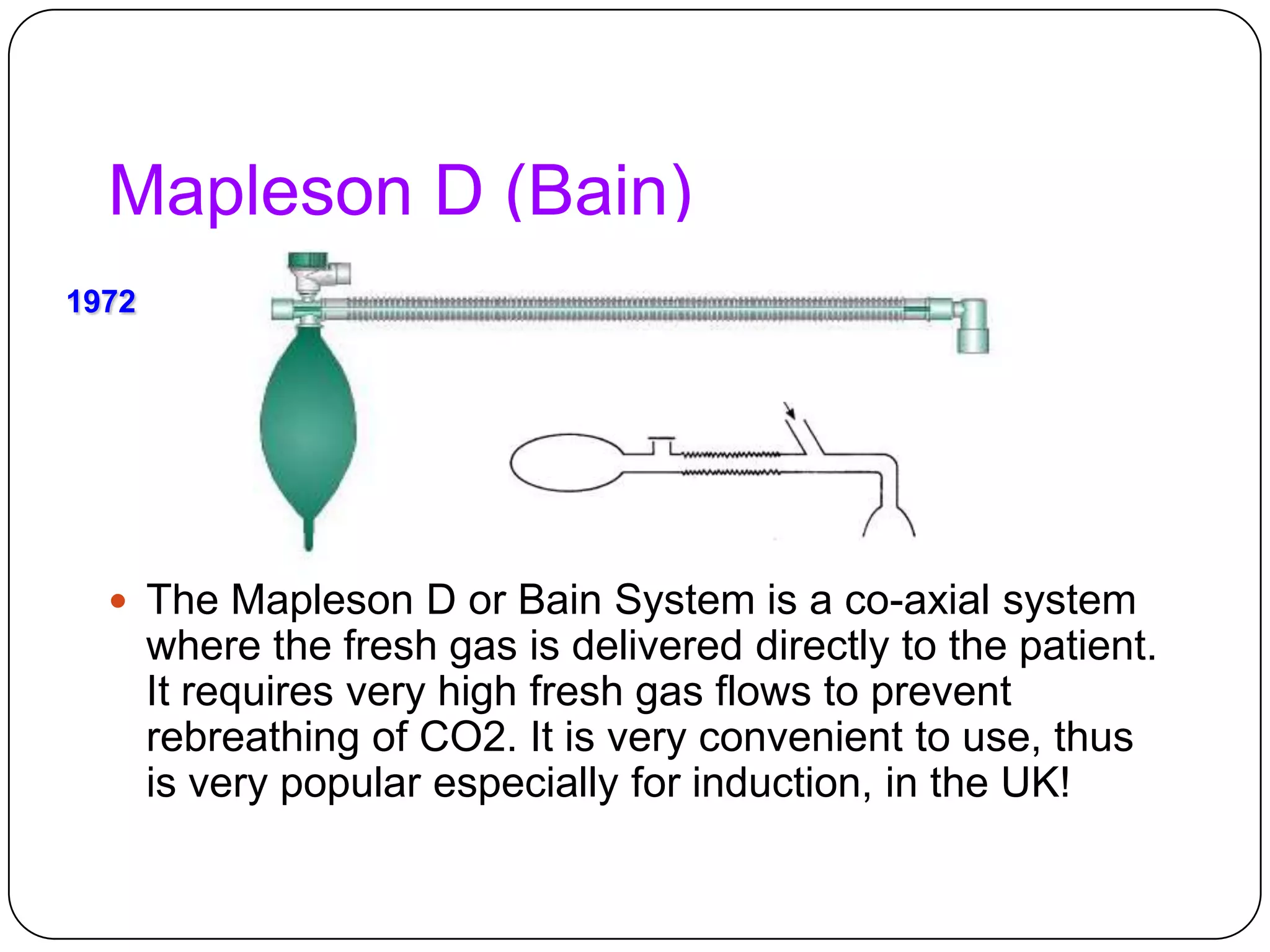
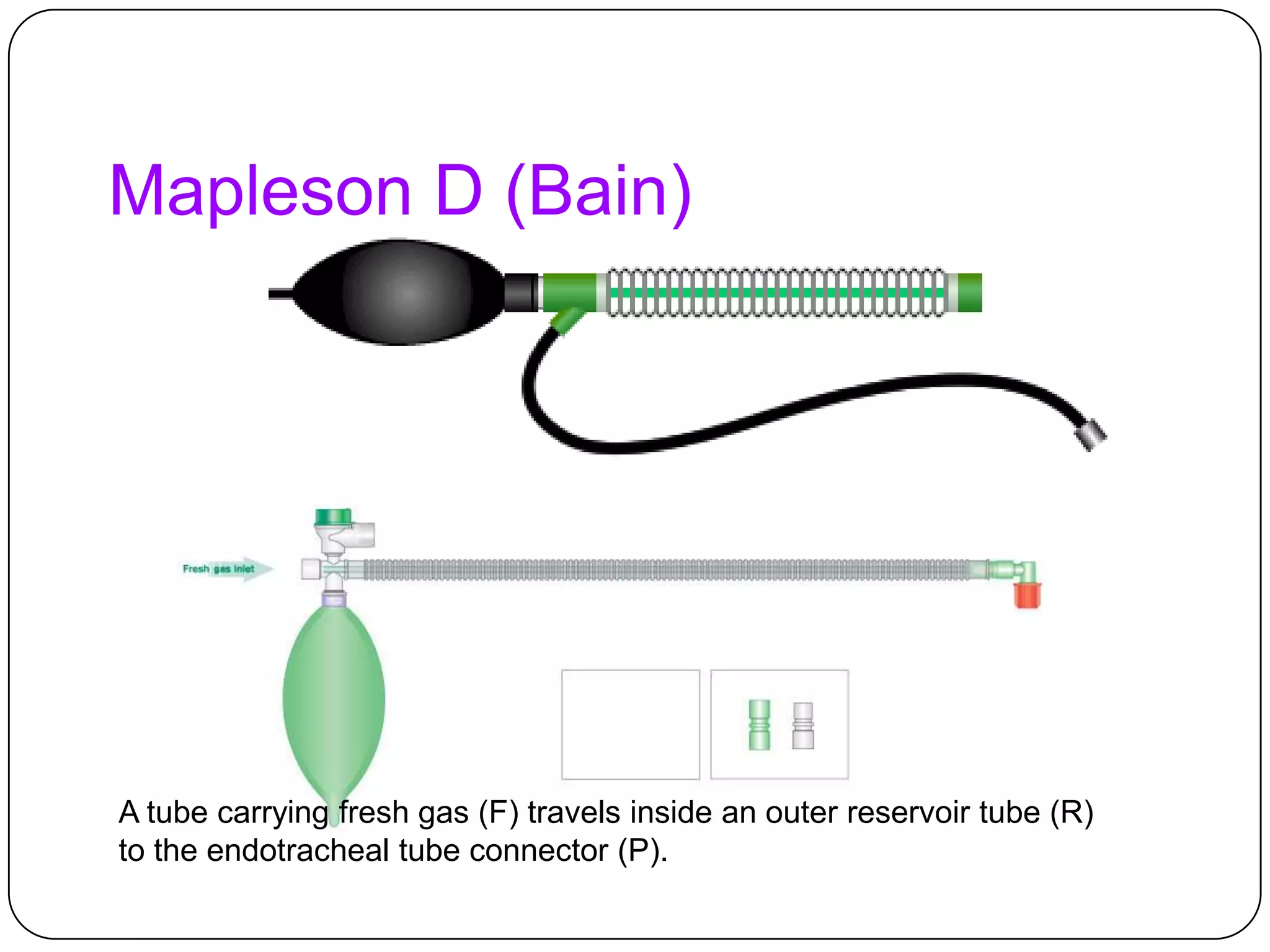
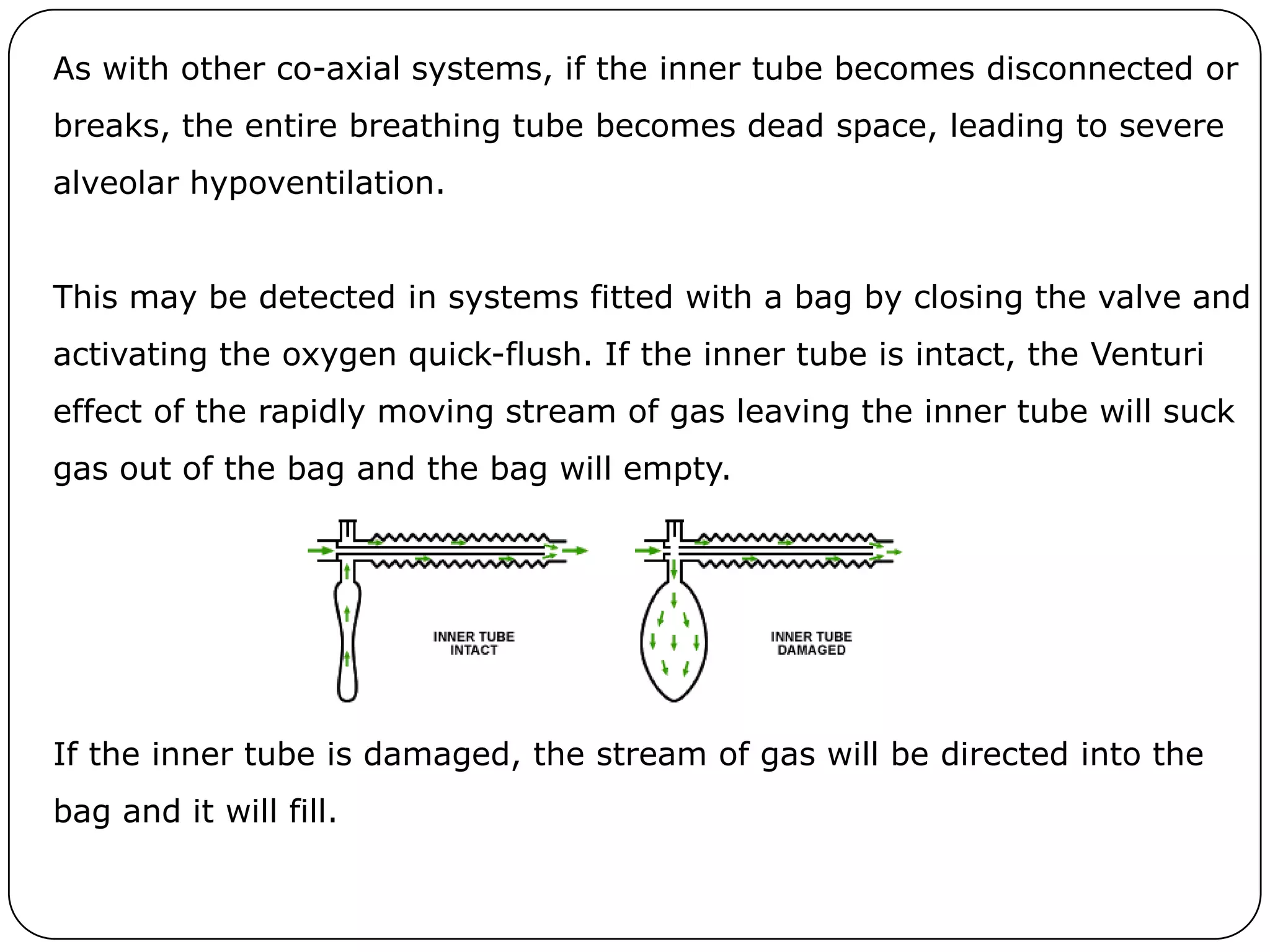
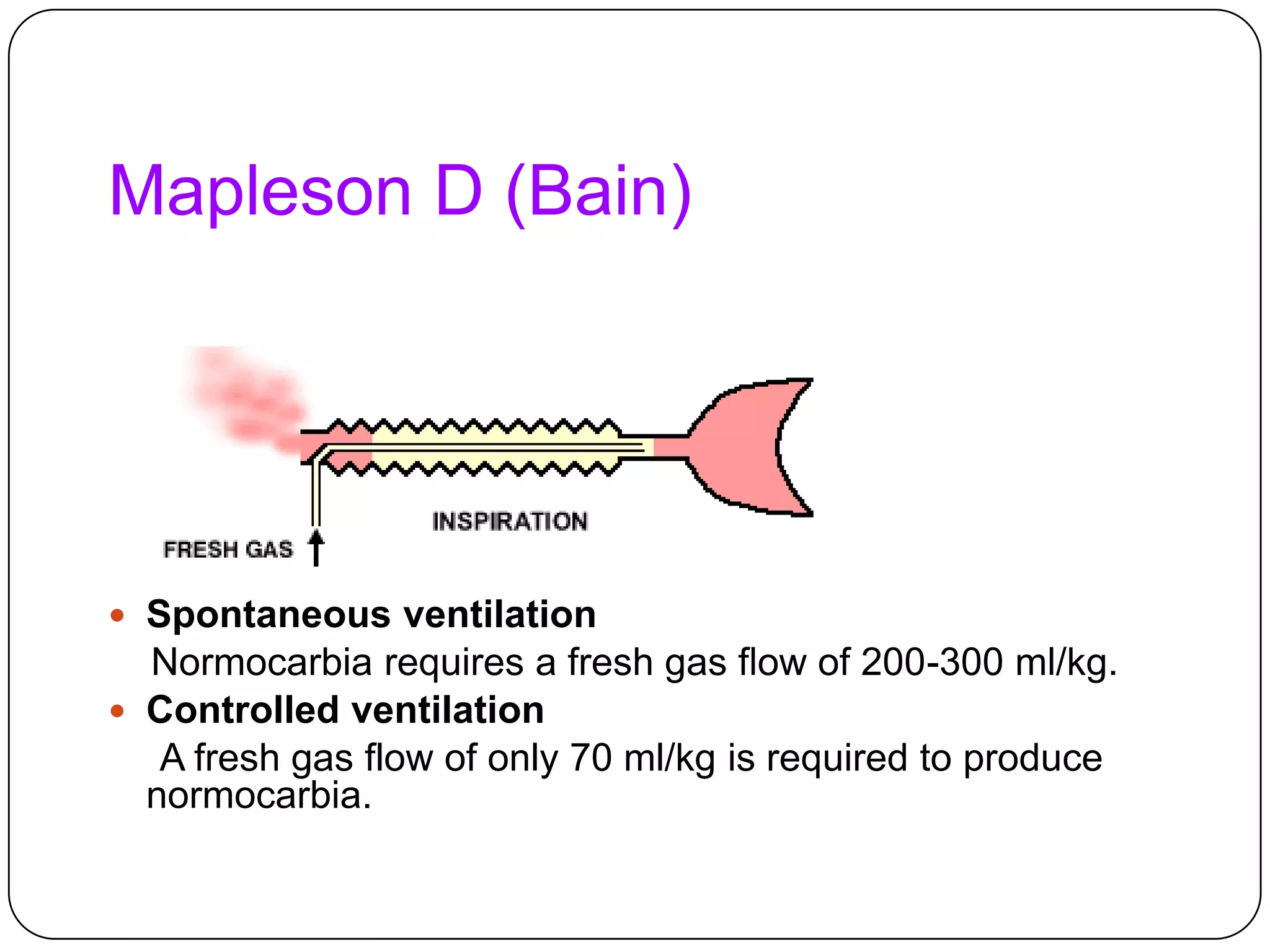
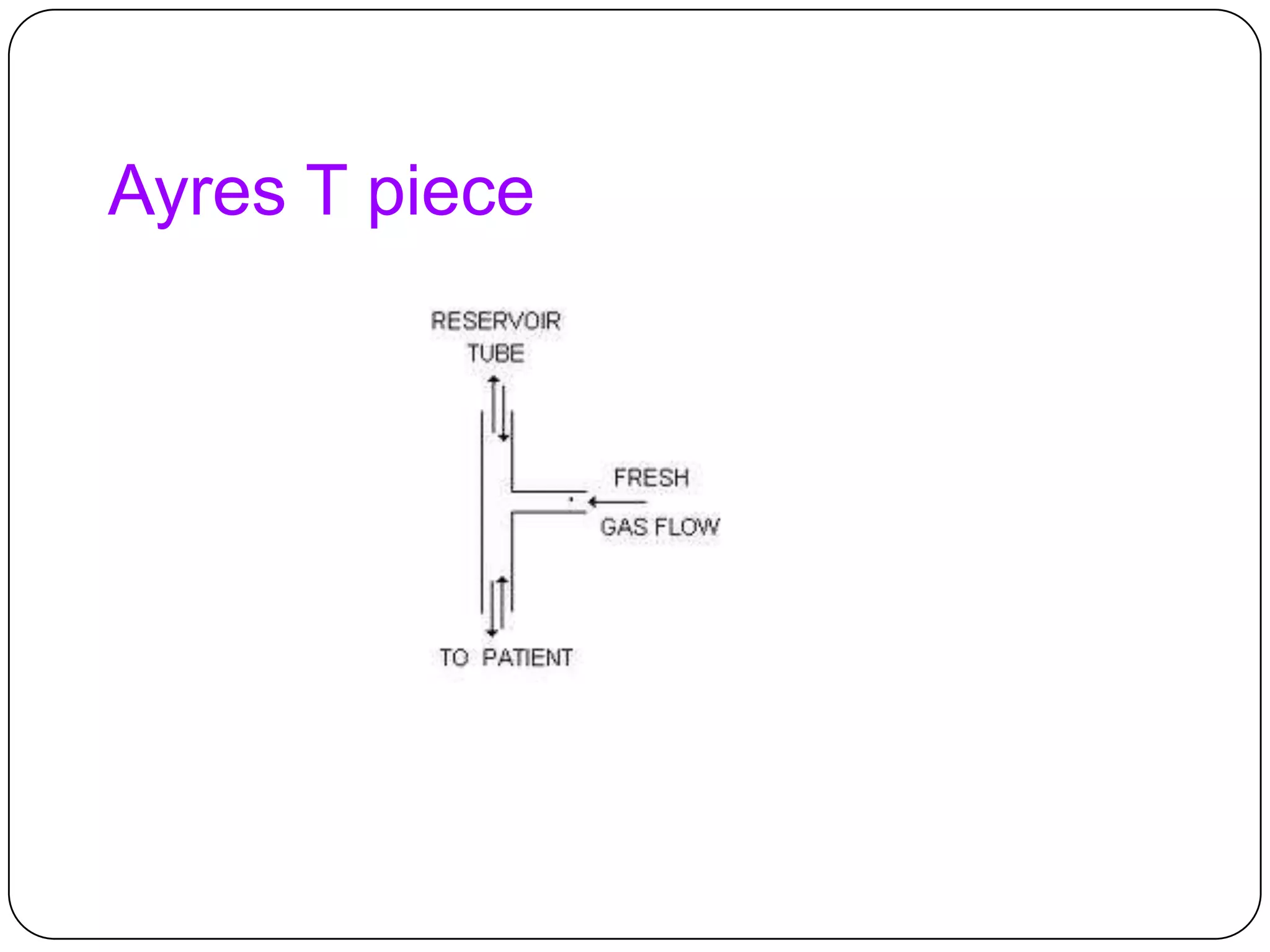
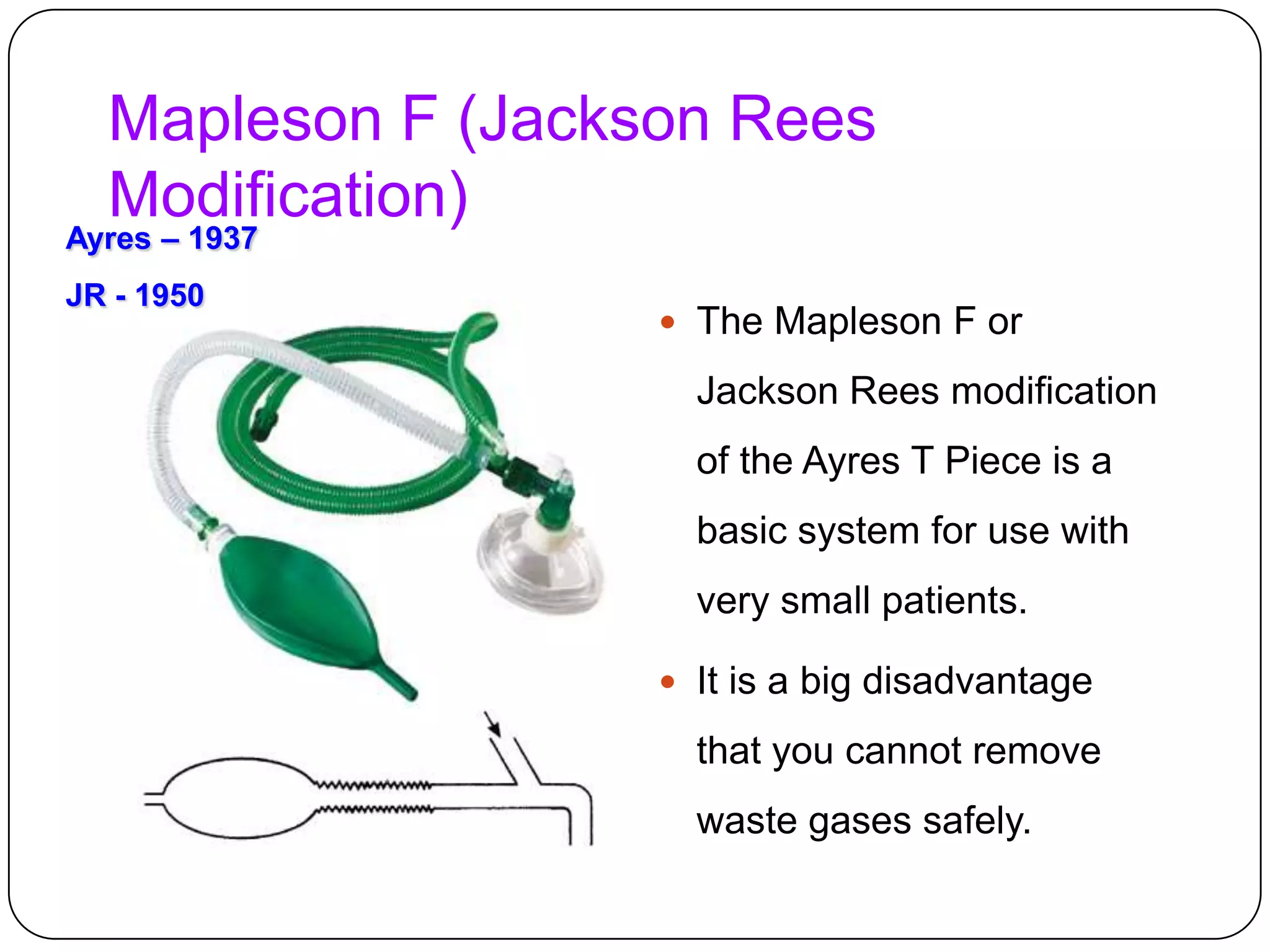
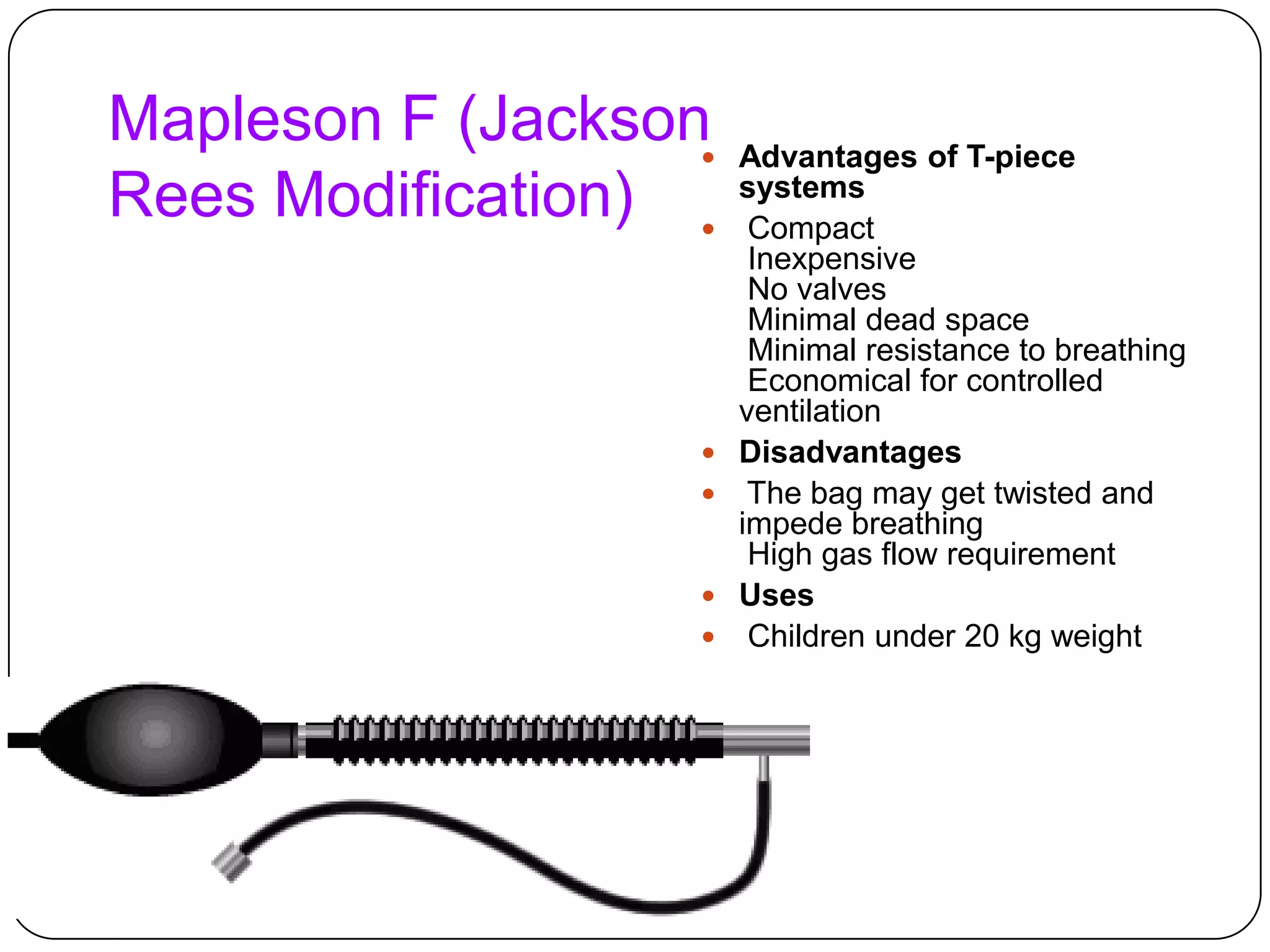
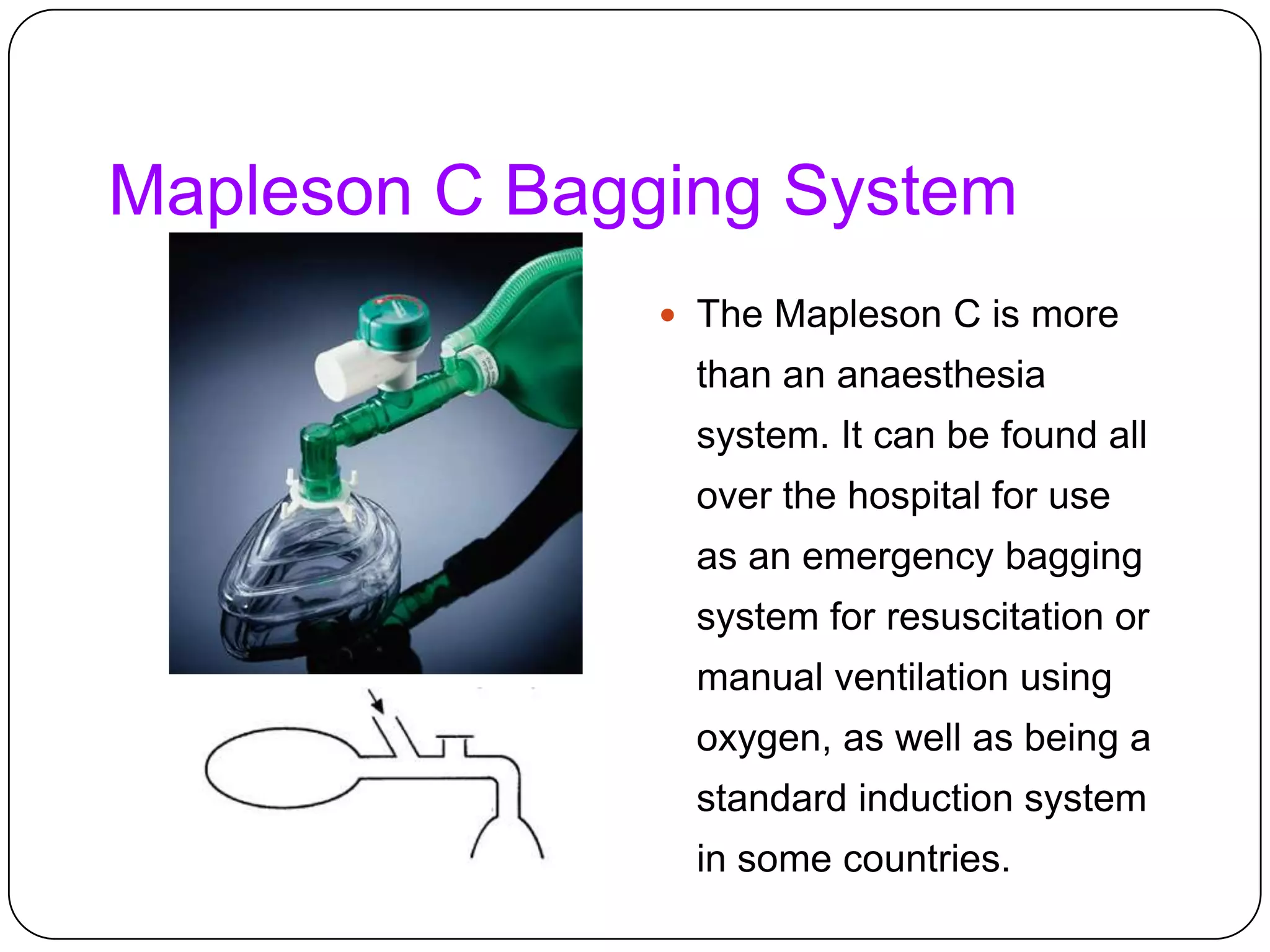
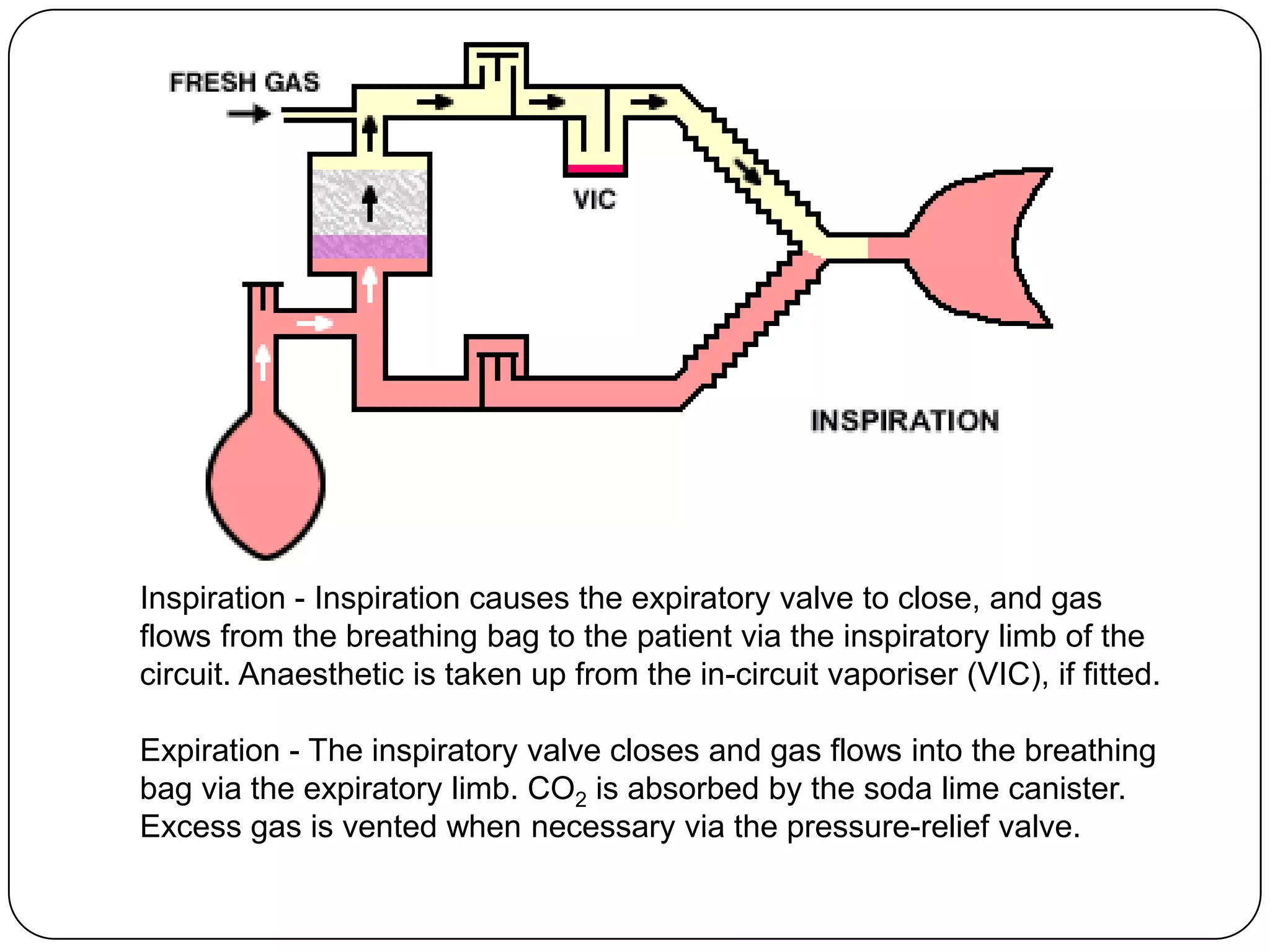
The document discusses different types of breathing circuits used in anesthesia. It begins by describing the basic components and functions of a breathing circuit, which delivers oxygen and anesthetic gases to patients while removing carbon dioxide. Circuits are classified as open, semi-open, semi-closed, or closed based on how exhaust gases are handled. Several specific circuit types are then outlined in detail, including the Mapleson A, Bain, Ayres T-piece, and Jackson-Rees systems. Key features and uses of each system are provided. Semi-closed circuits are explained as using a carbon dioxide absorber to remove carbon dioxide from exhaled gases so they can be rebreathed, allowing for lower fresh gas flow rates than open systems