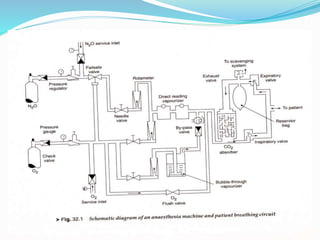
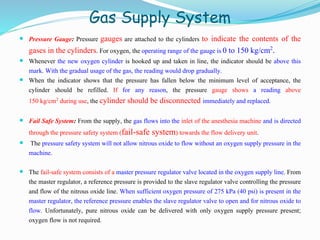
An anesthesia machine uses gas supply and delivery systems to provide precise mixtures of medical gases like oxygen, nitrous oxide, and anesthetic vapors to patients during surgery. Key components include connections to hospital gas lines, reserve gas cylinders, flow meters, vaporizers, and monitors. Modern machines also integrate ventilators and monitors for vital signs. Anesthesia machines allow anesthesiologists to safely induce and maintain general anesthesia, while carefully controlling gas concentrations and supporting patient breathing.