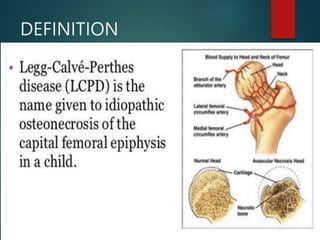
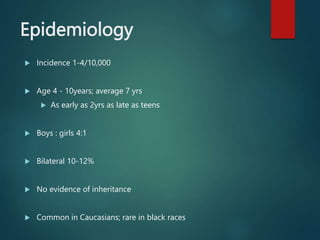
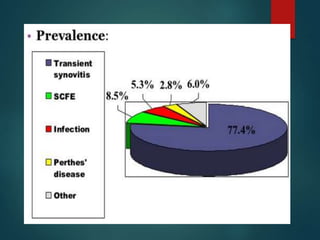
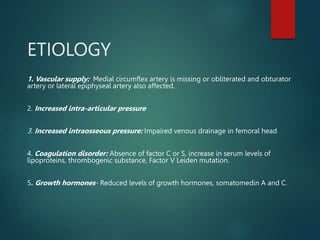
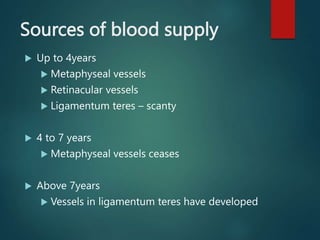
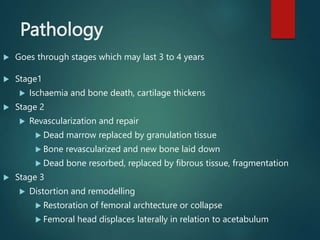
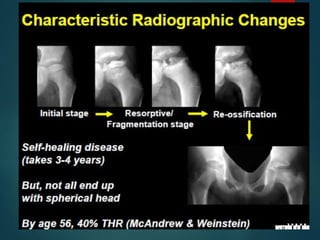
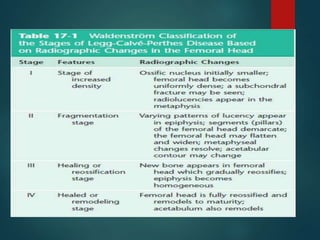
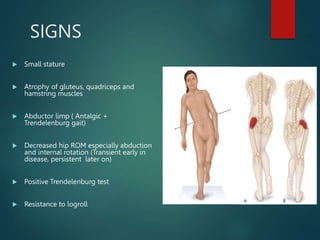
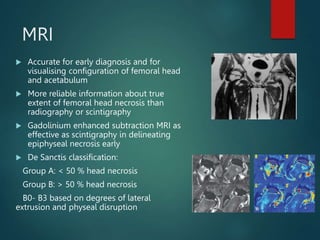
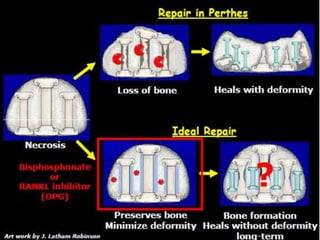
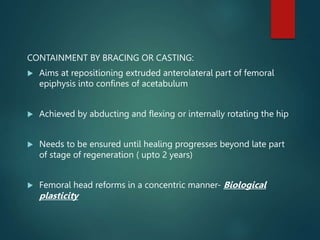
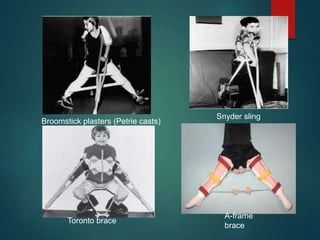
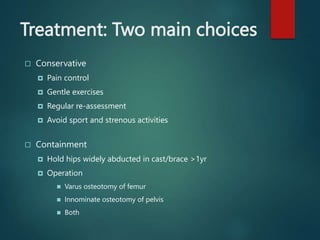
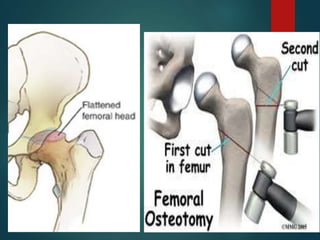
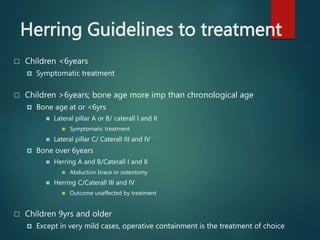
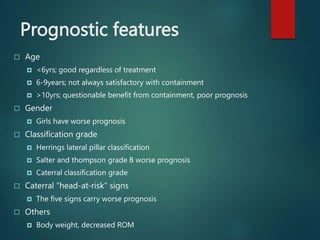
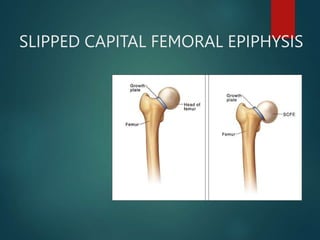
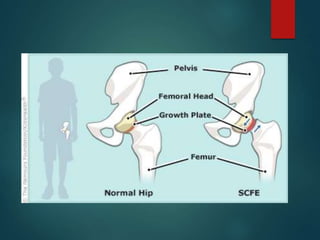
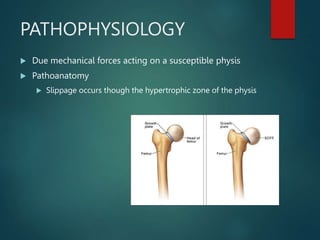
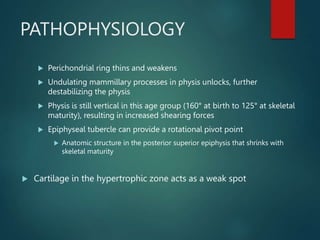
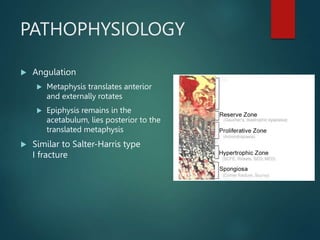
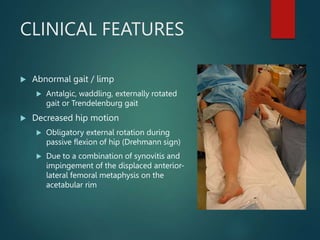
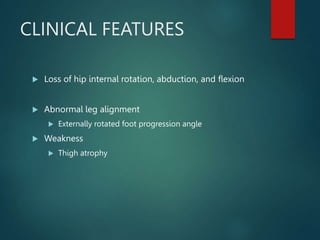
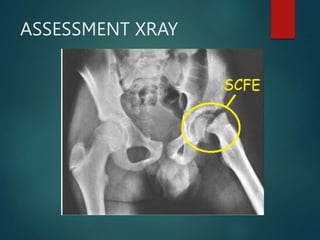
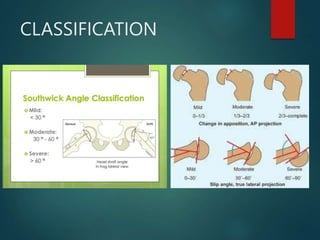
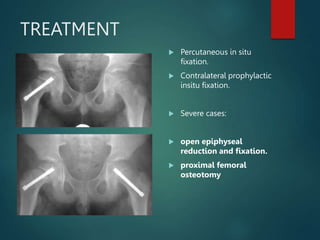
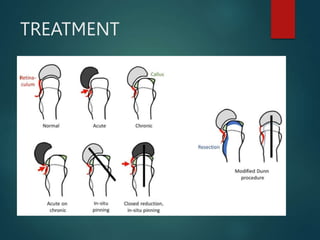
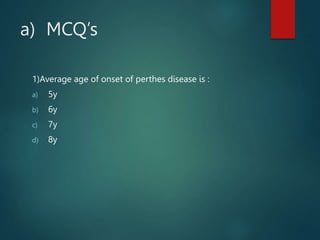
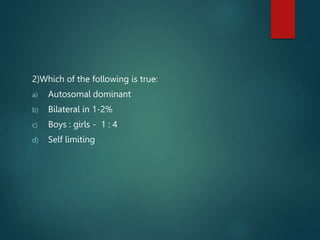
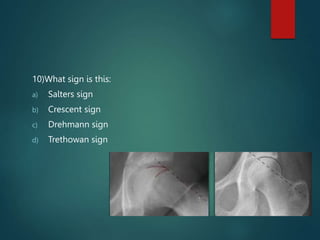
Perthes disease and slipped capital femoral epiphysis (SCFE) are conditions affecting the hip joint in children. Perthes disease causes temporary loss of blood supply to the femoral head, leading to bone death. It most commonly affects boys aged 4-10 years. SCFE is caused by slippage of the femoral epiphysis and is associated with obesity in puberty. Both can be diagnosed on x-ray and treated conservatively with bracing or surgically in severe cases to prevent joint damage.