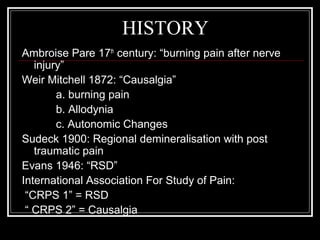
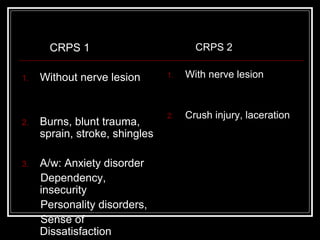
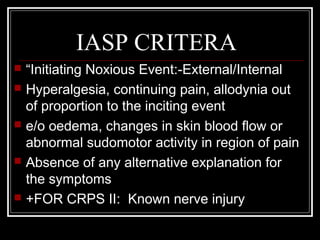
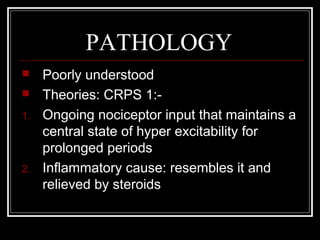
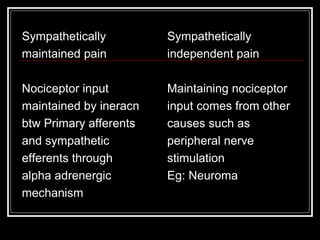
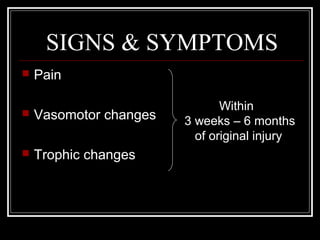
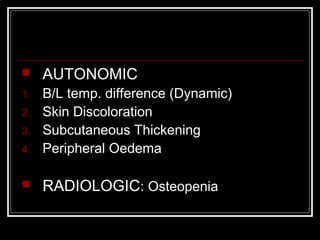
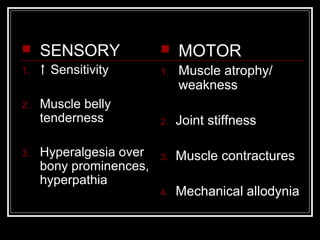
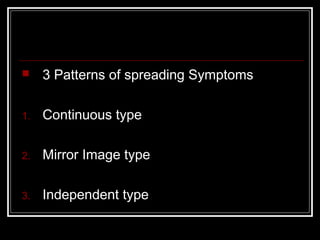
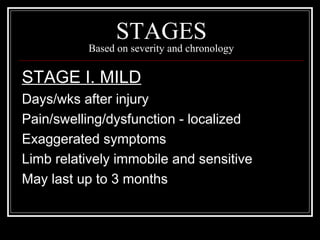
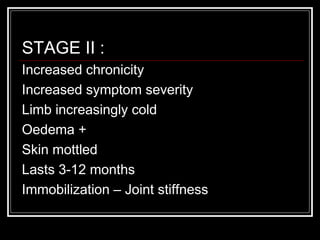
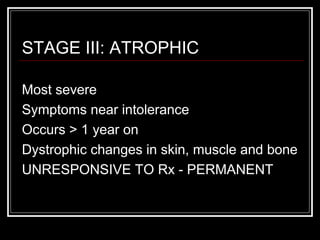
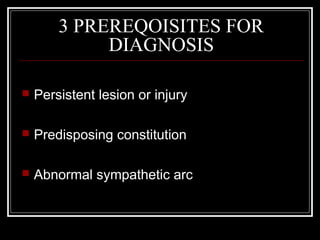
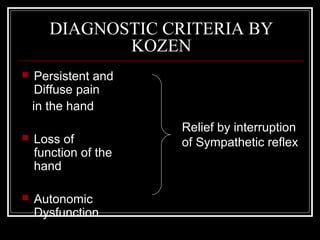
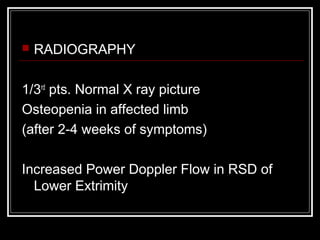
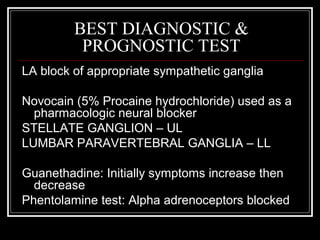
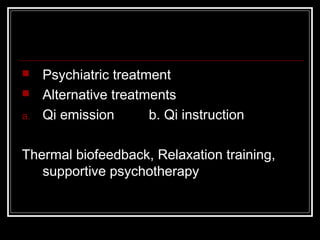
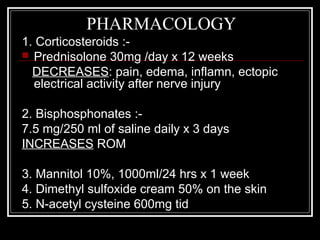
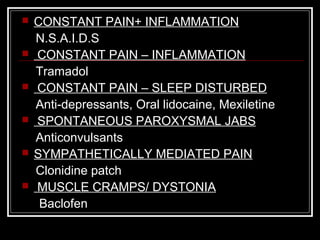
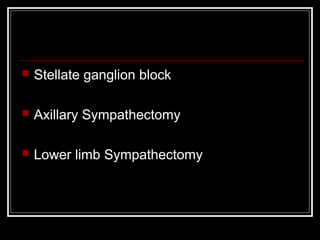
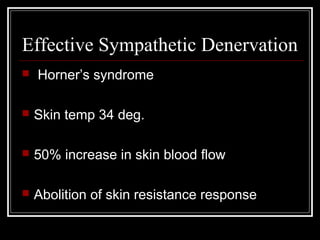
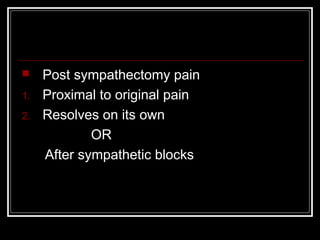
Reflex Sympathetic Dystrophy (RSD), now known as Complex Regional Pain Syndrome (CRPS), is a chronic pain condition that usually affects an extremity like an arm or leg following an injury. It causes ongoing pain that is out of proportion to the original injury and involves changes in skin, bone, and blood vessels in the affected area. CRPS is classified into two types depending on whether there is confirmed nerve damage present. Treatment involves a multidisciplinary approach including medications, physical therapy, sympathetic nerve blocks, and in severe cases, surgical sympathectomy to relieve pain.