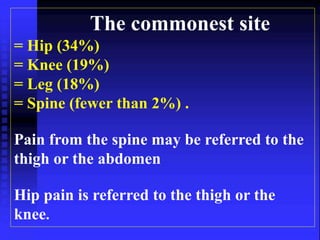
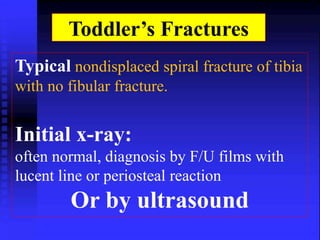
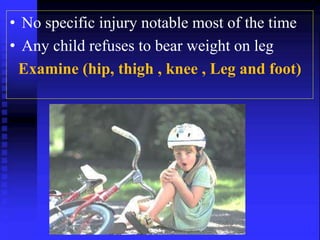
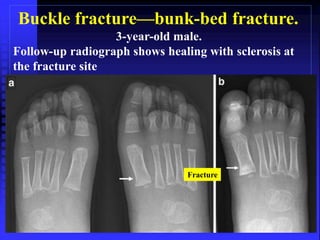
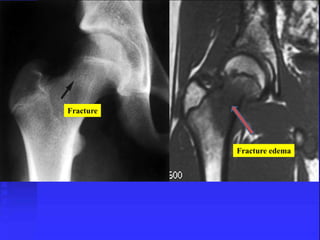
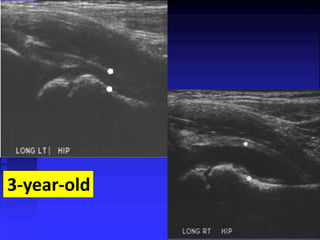
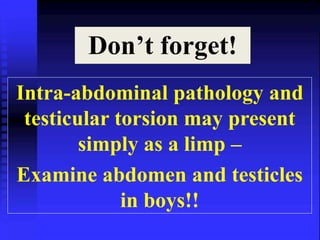
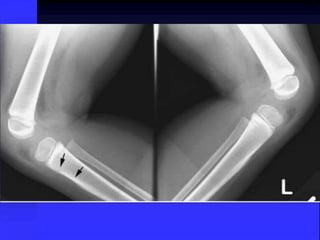
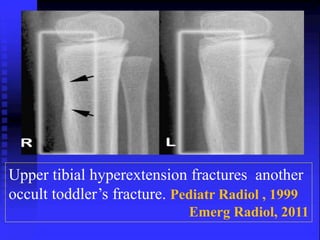
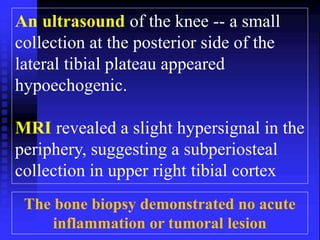
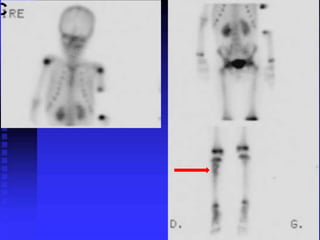
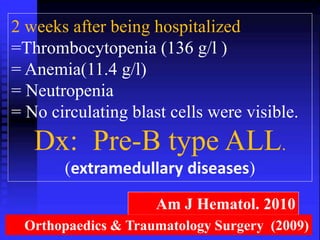
1) A 3-year-old male presented with right knee pain and inability to bear weight after being kicked. Initial x-rays were negative but symptoms persisted.
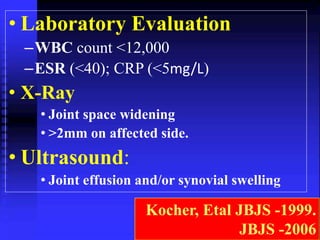
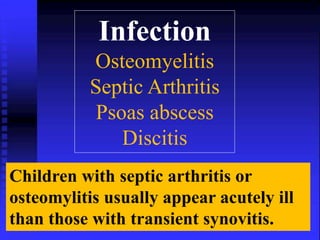
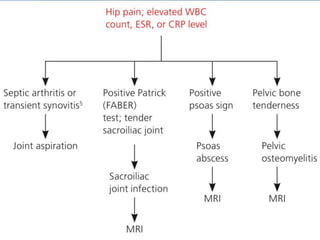
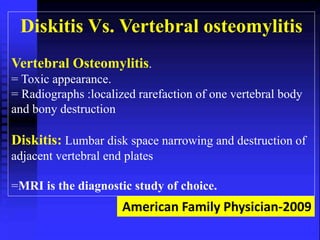
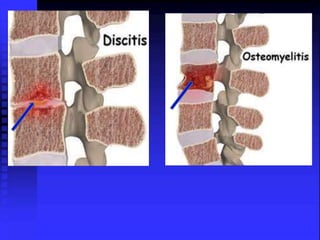
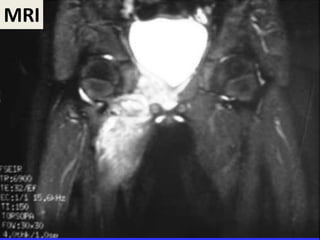
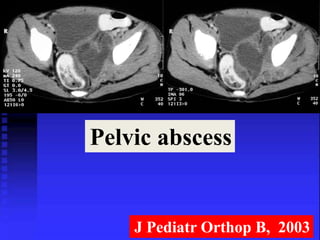
2) A 6-year-old girl presented with a 3-week history of right hip pain and fever 10 weeks prior. Exam found increased lumbar lordosis and hip tenderness. Tests found elevated ESR and CRP. MRI and biopsy revealed pelvic osteomyelitis.
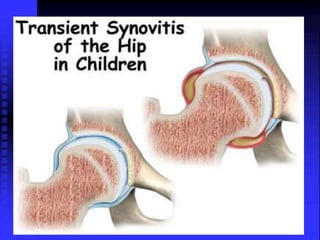
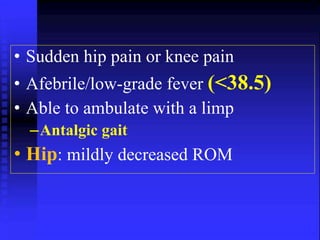
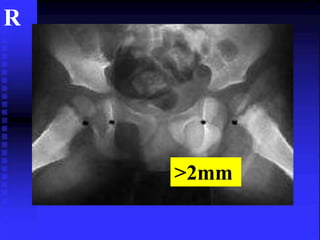
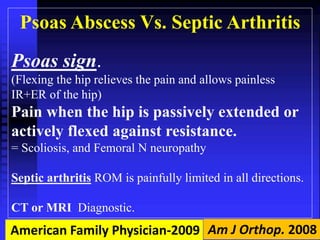
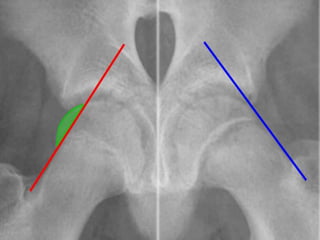
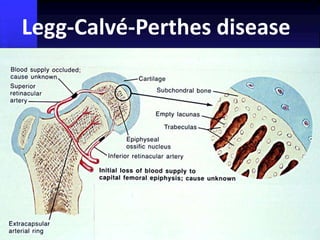
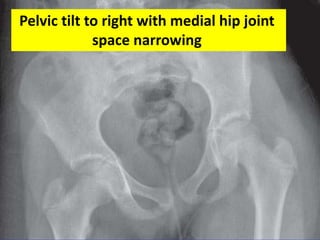
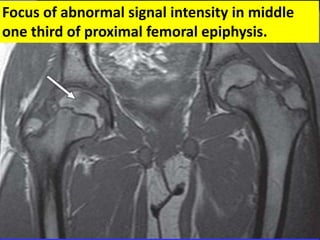
3) A 5-year-old male reported right hip pain after falling down stairs, though he was able to play basketball with no pain initially. Exam found normal ROM but pain with movement of the right leg. Radiographs of the pelvis