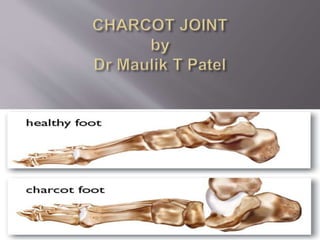
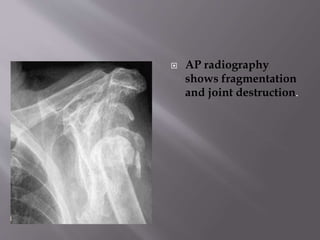
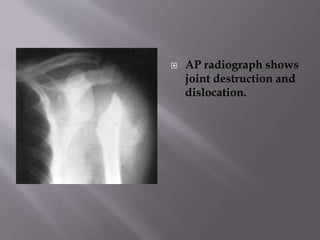
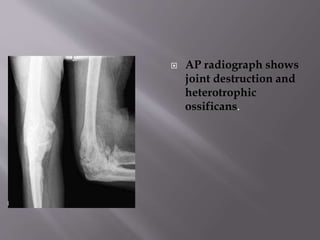
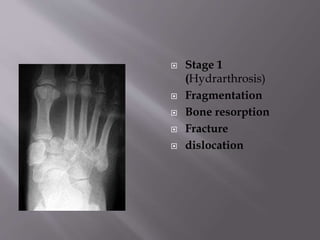
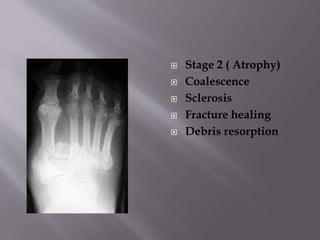
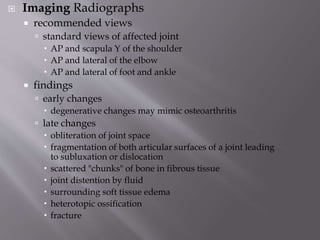
Charcot joint disease, first described by Jean-Martin Charcot in 1868, is a progressive joint condition often misdiagnosed, primarily affecting the lower limbs and linked to neuropathy, especially from diabetes. Imaging techniques like X-rays and MRI are critical for diagnosis, distinguishing it from conditions like osteomyelitis, which shows different scan results. Treatment includes rest and immobilization, with surgical options available in non-inflammatory stages.