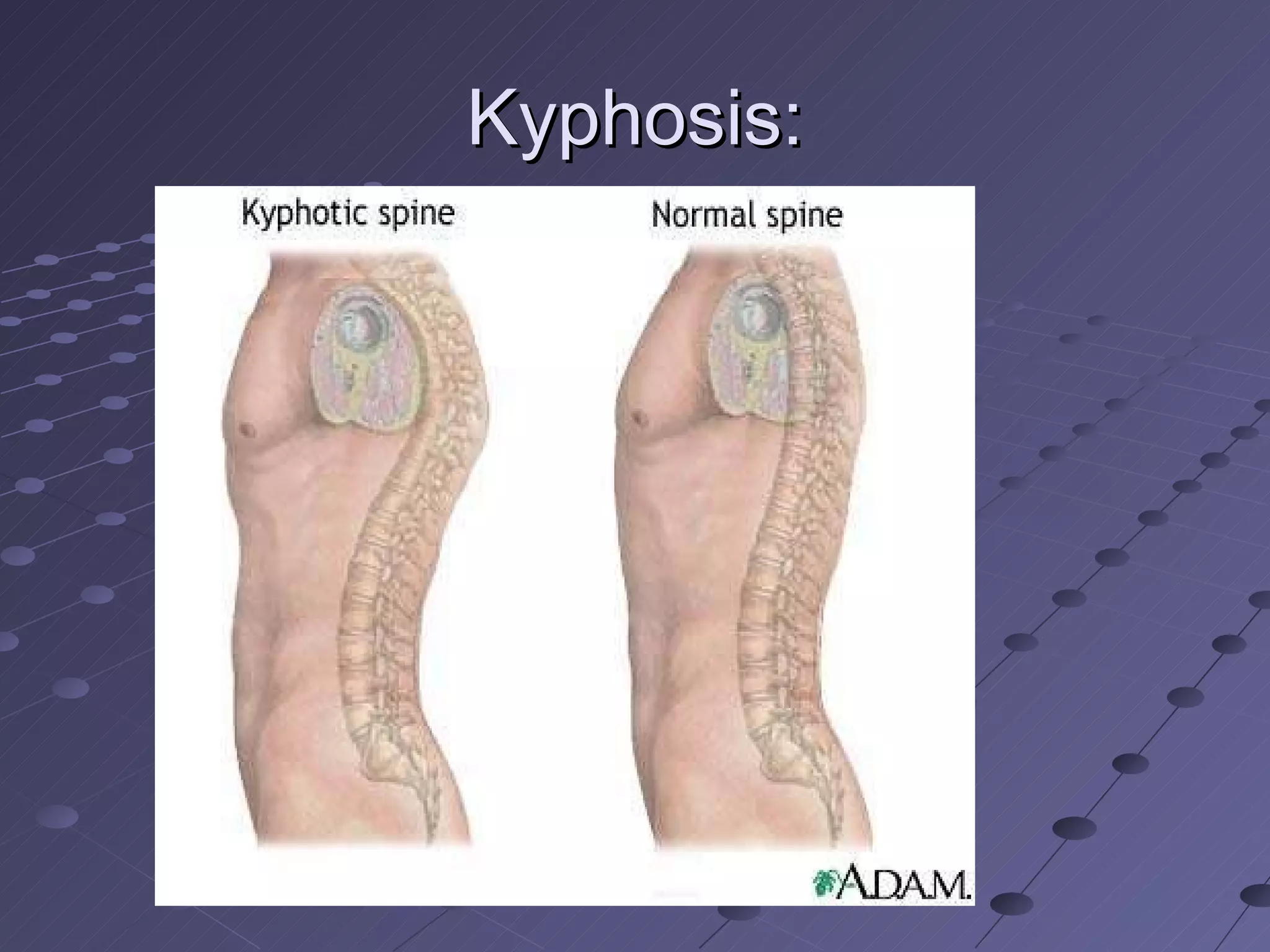
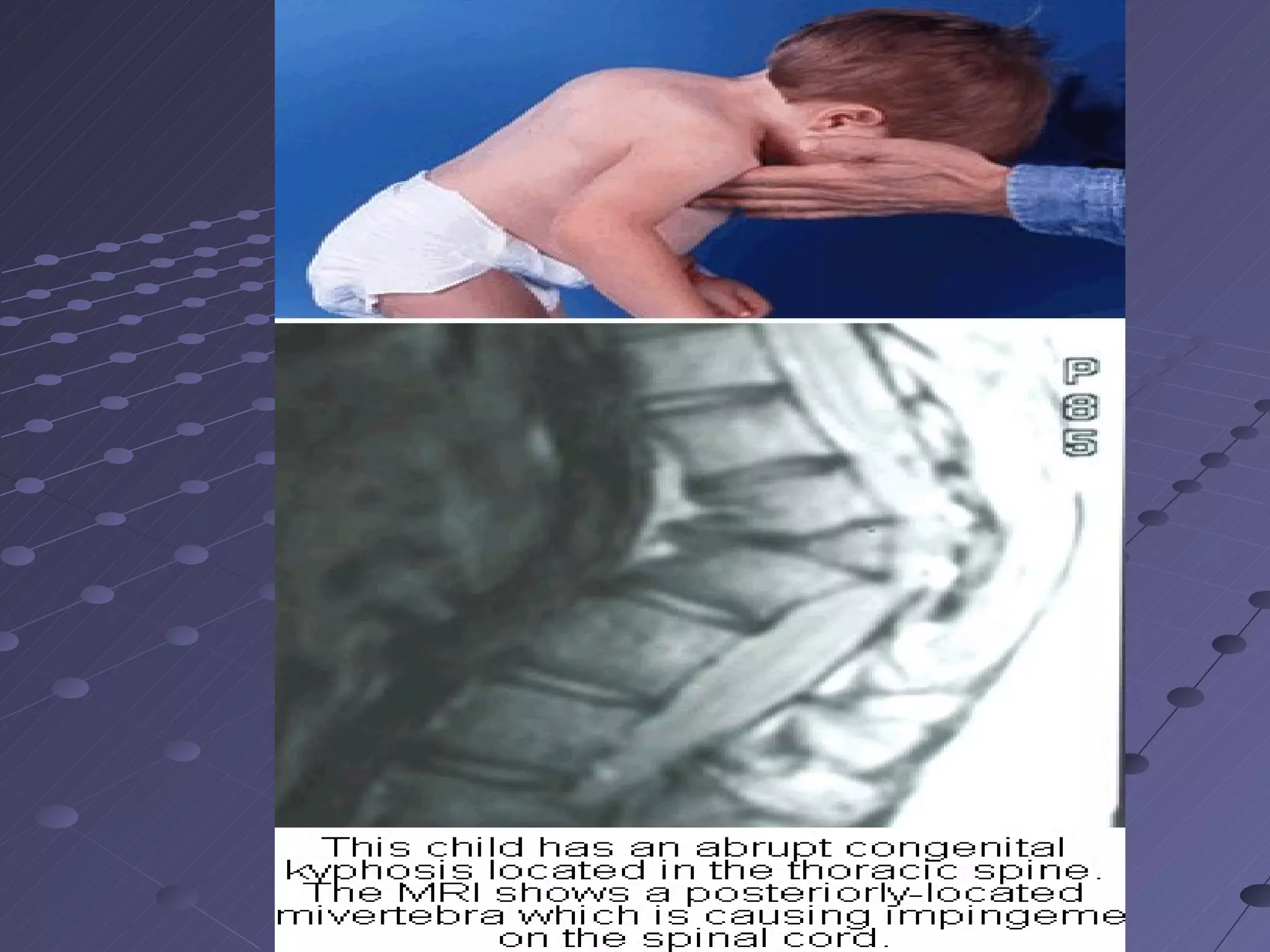
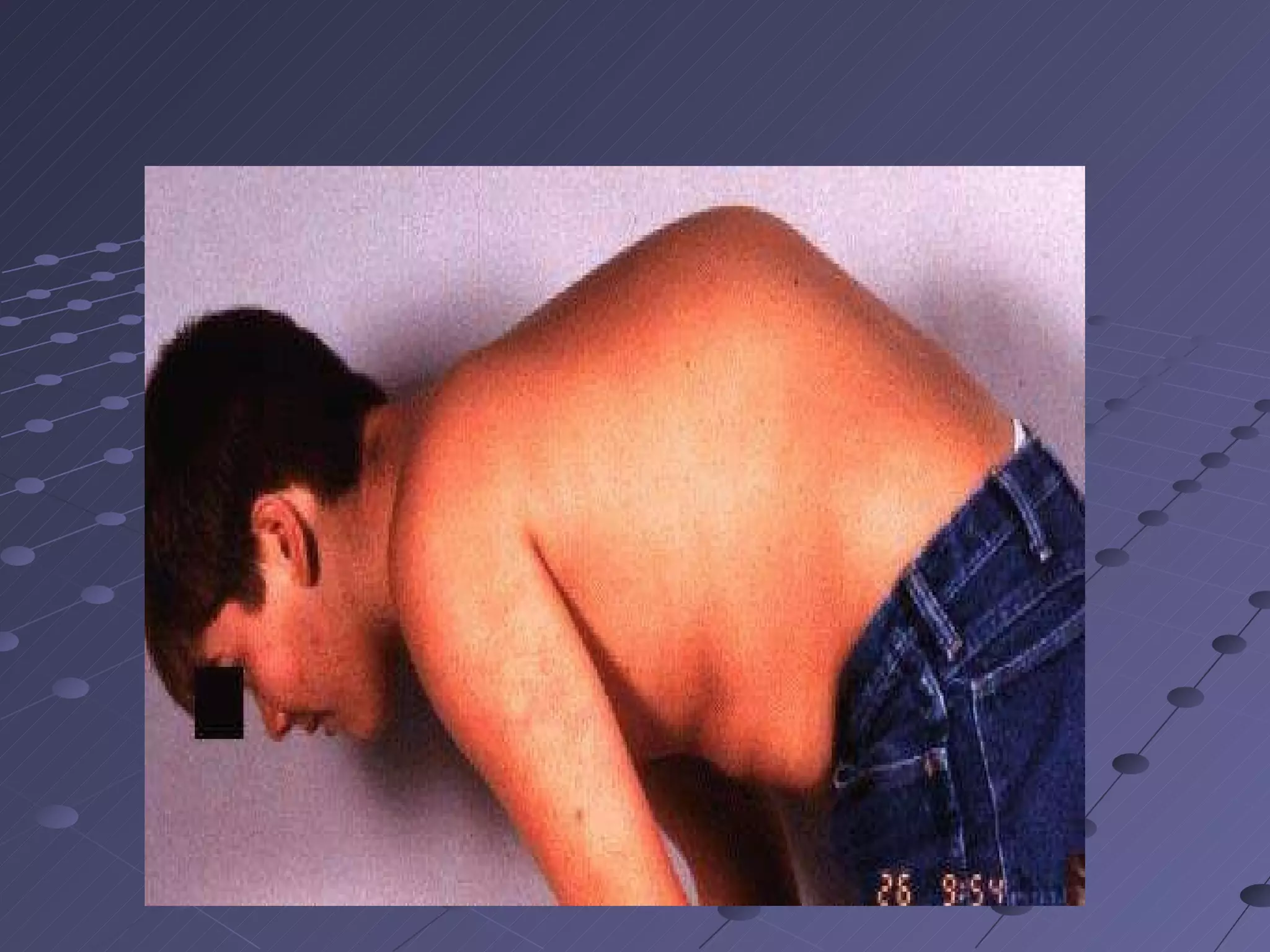
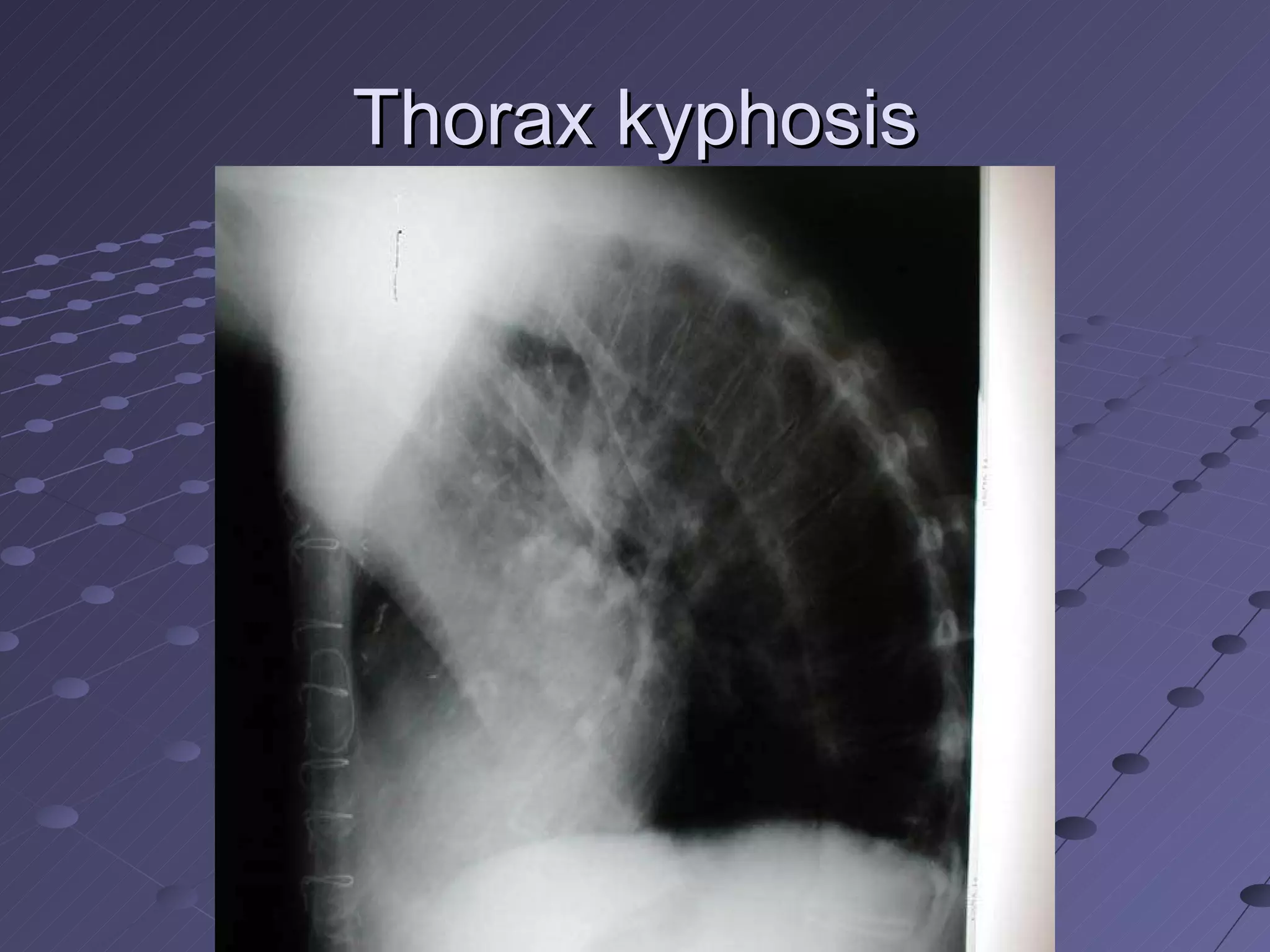
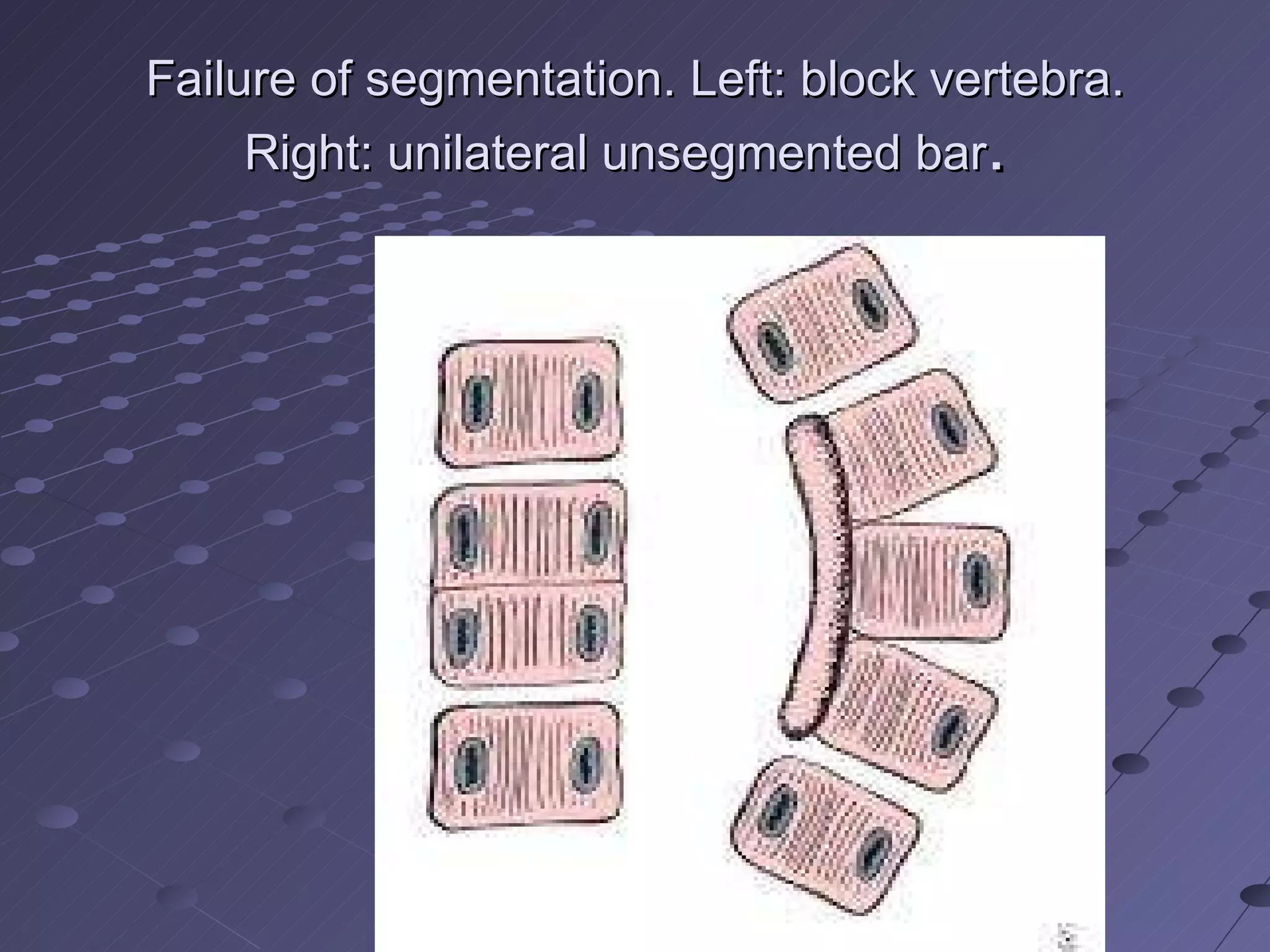
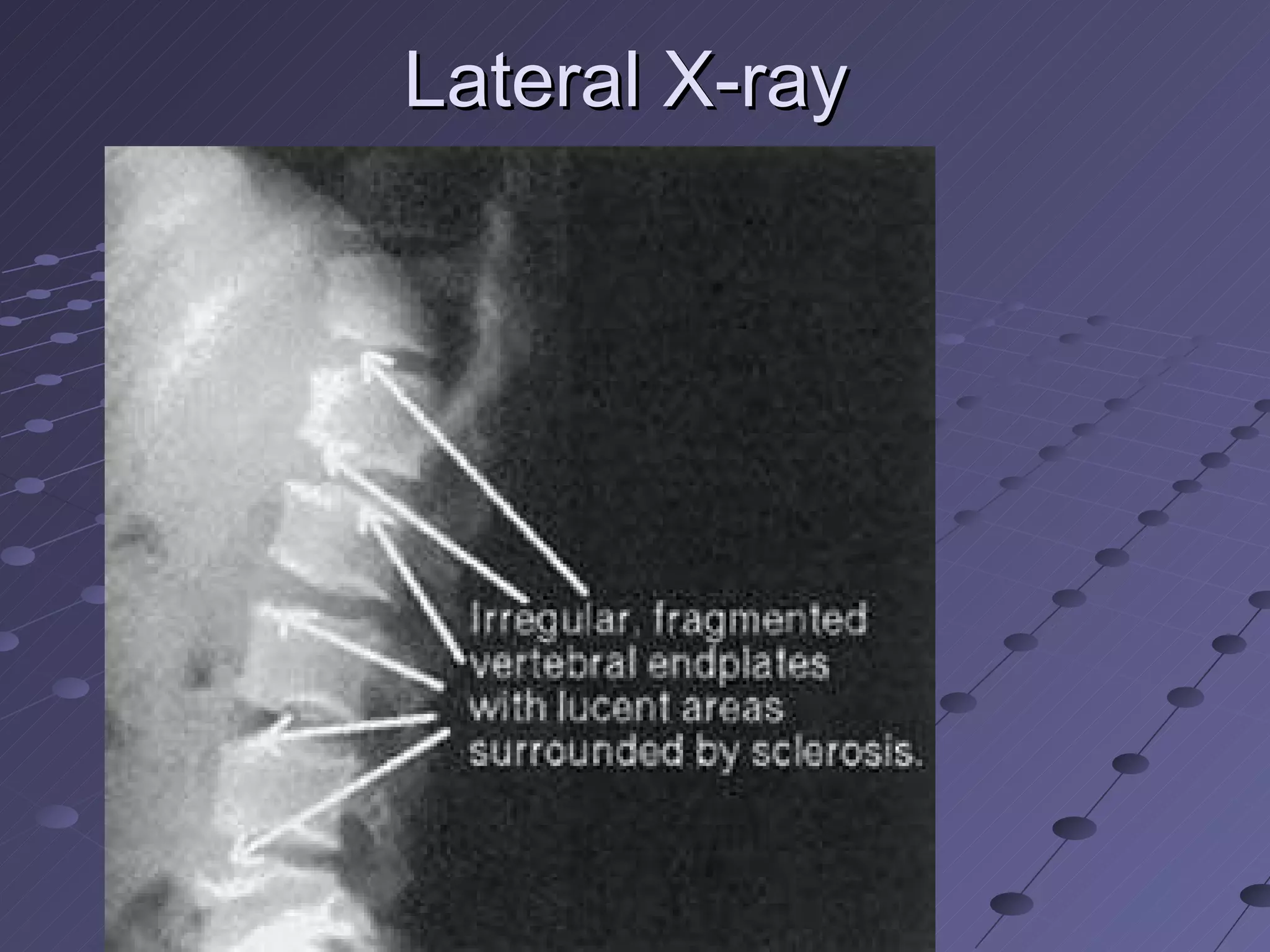
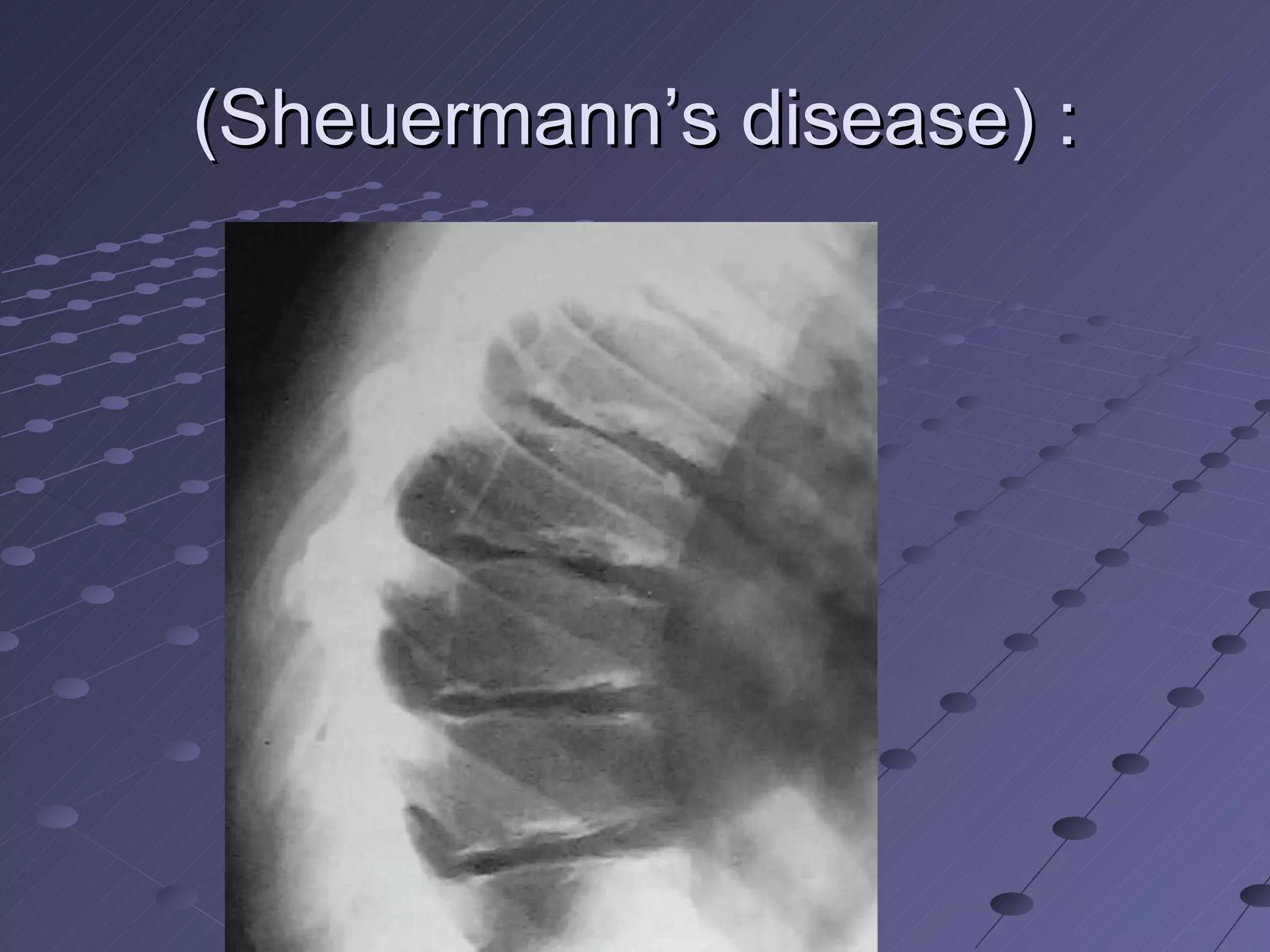
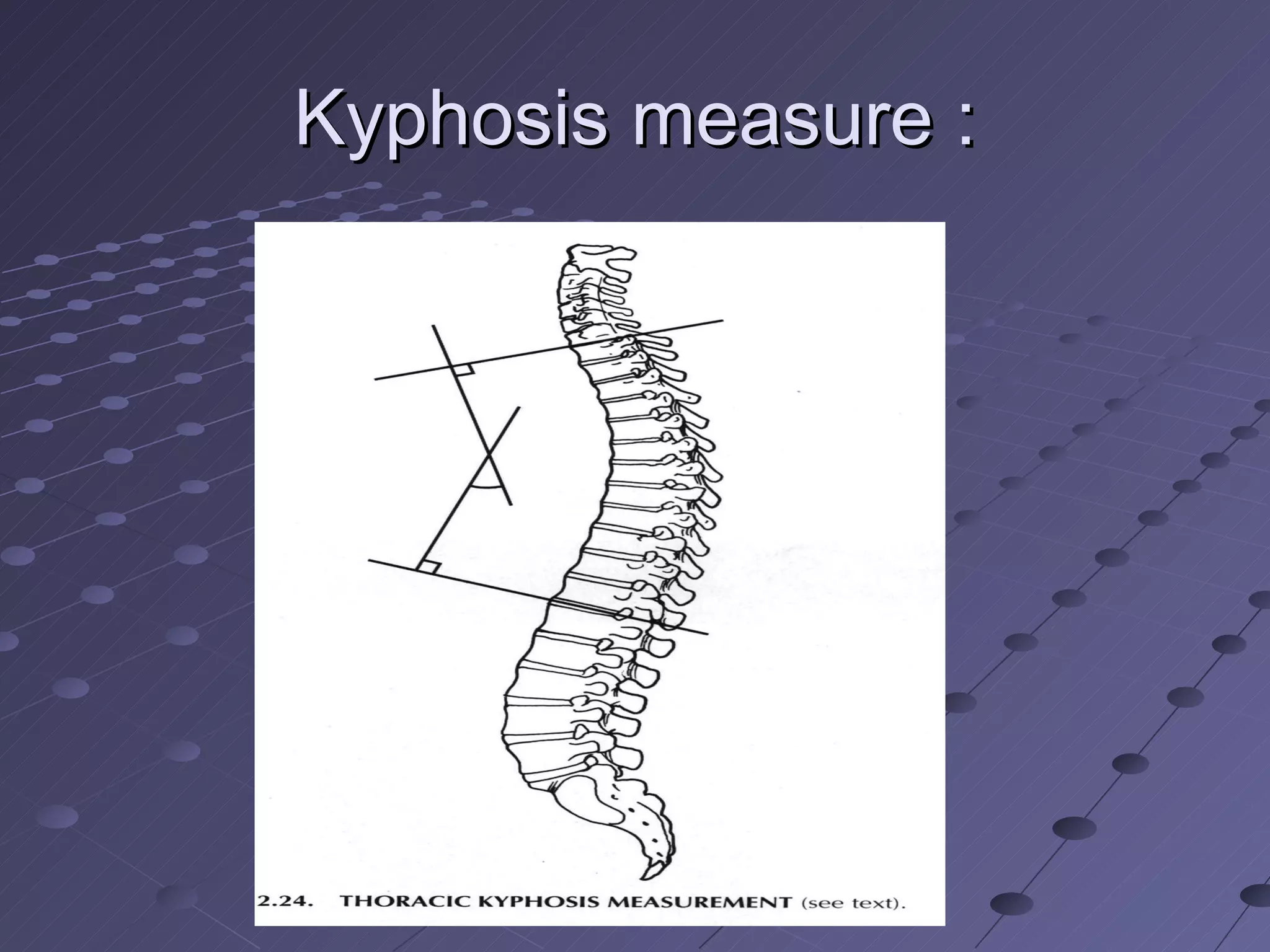
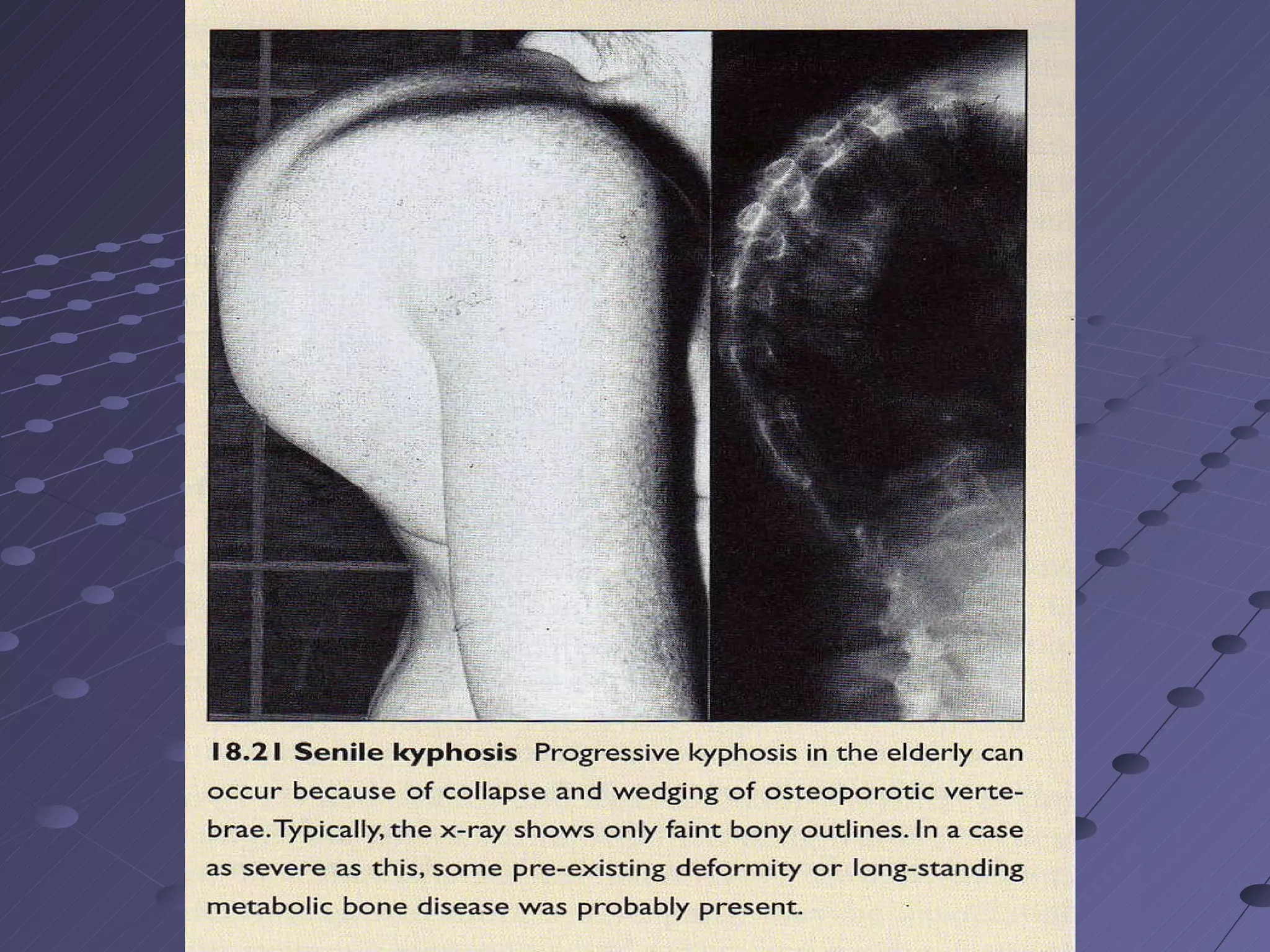
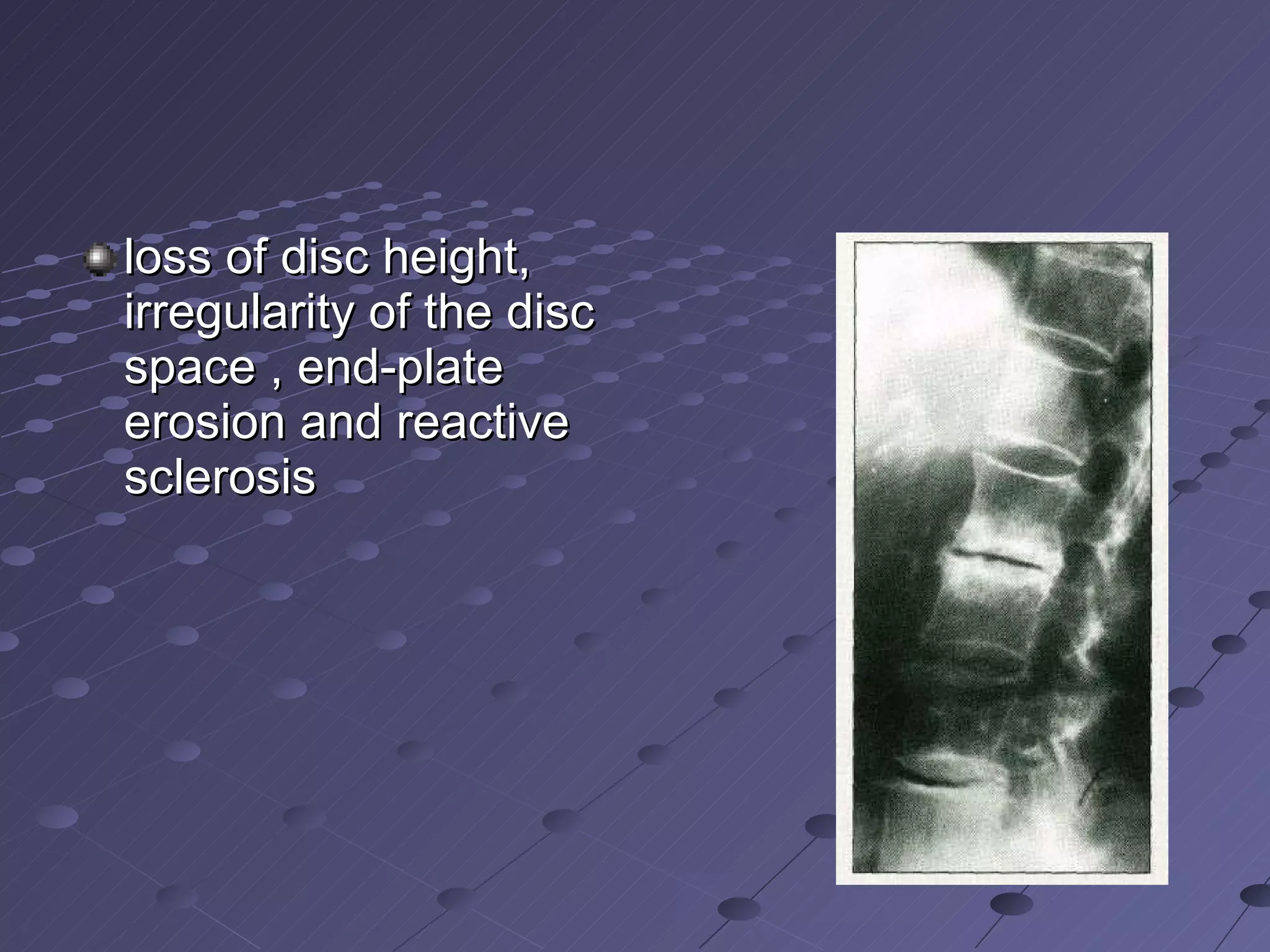
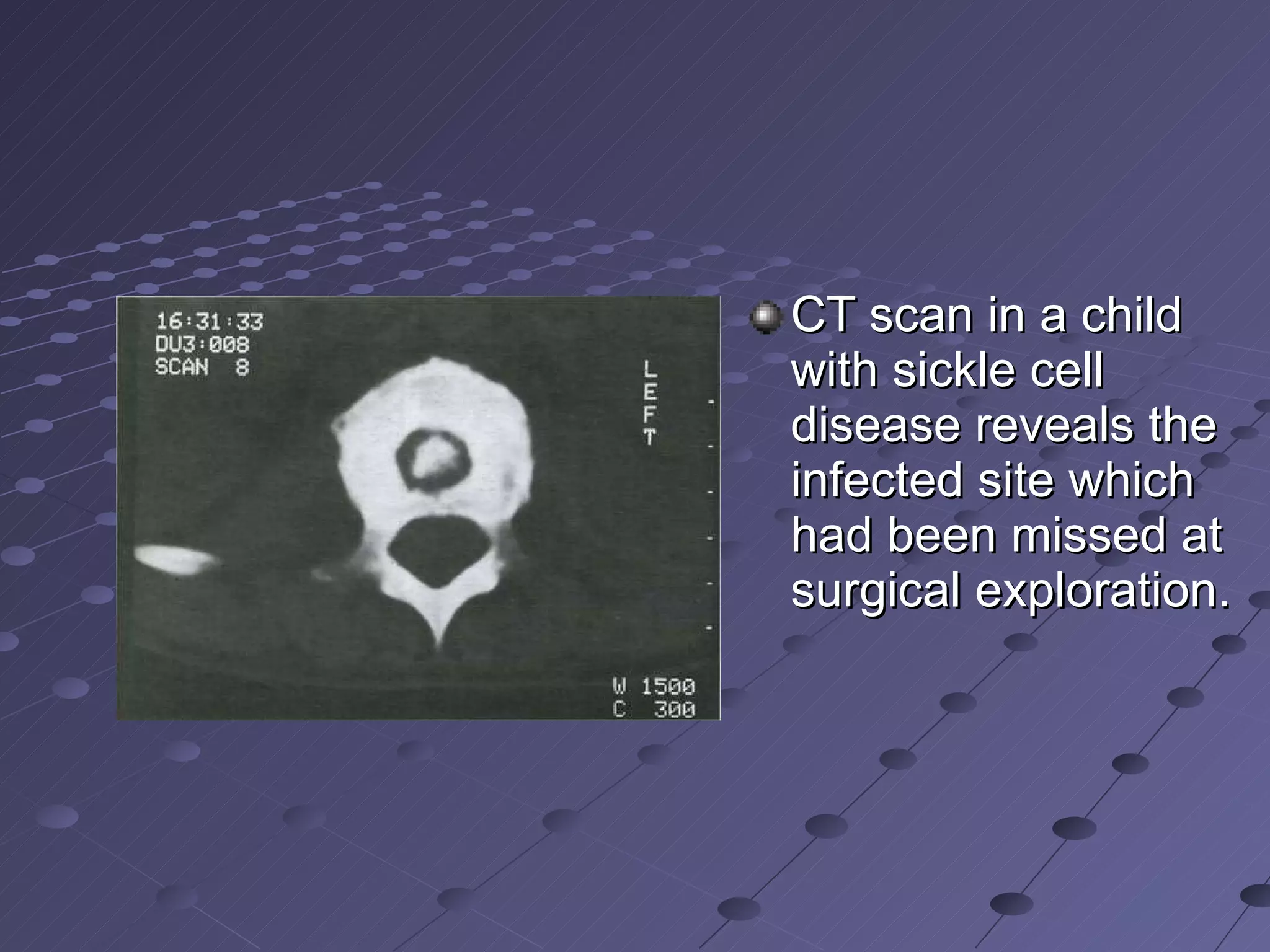
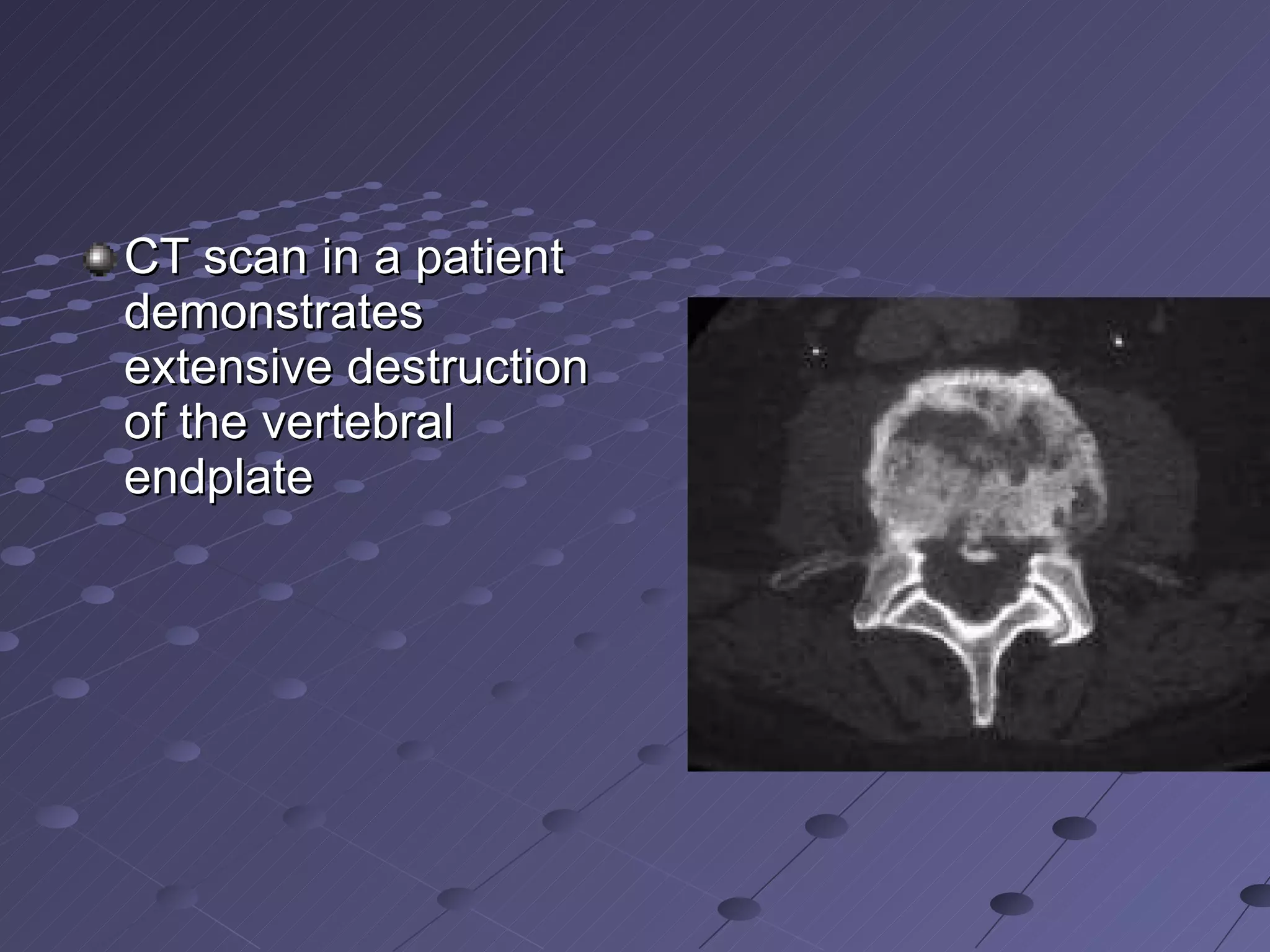
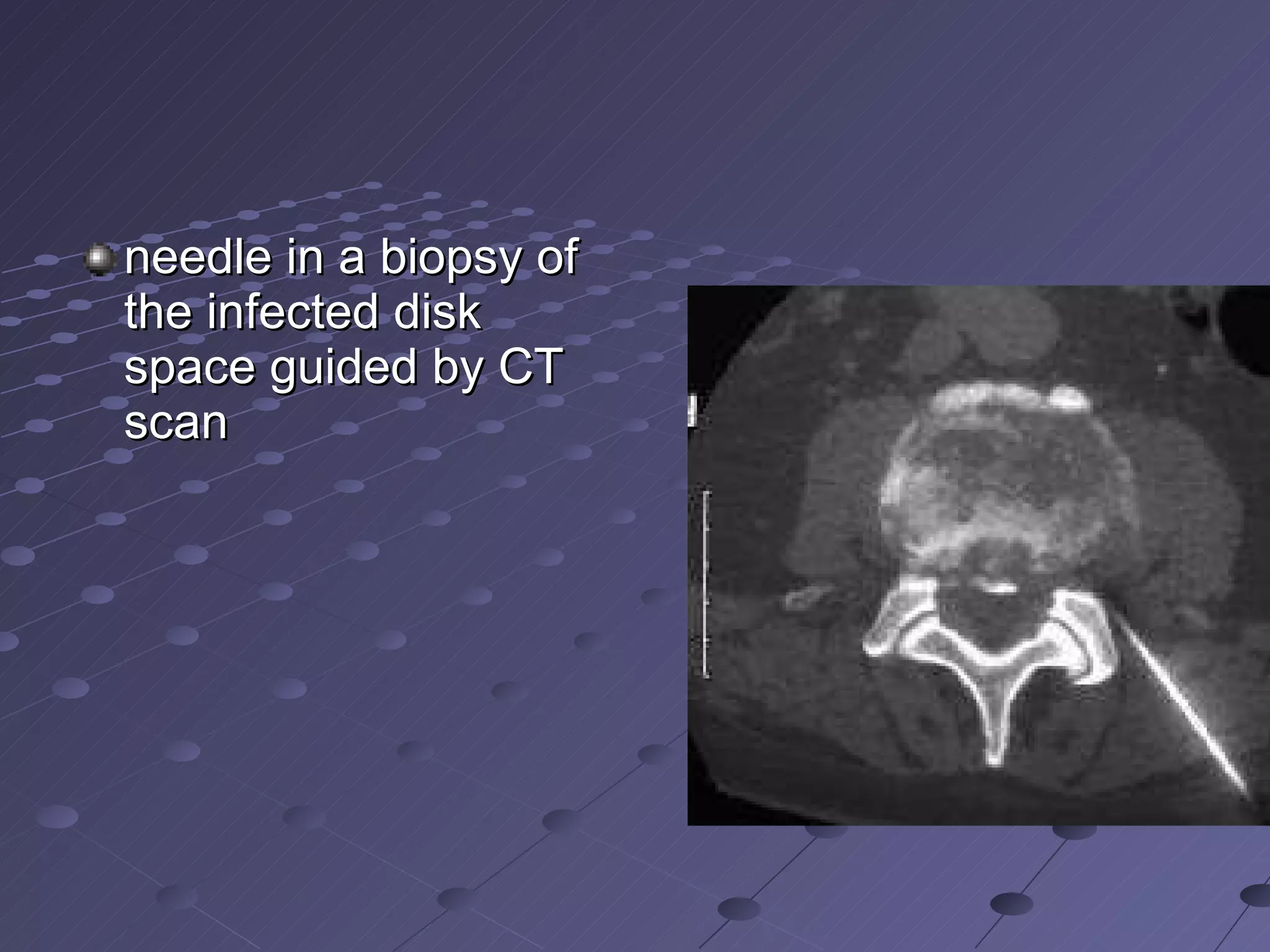
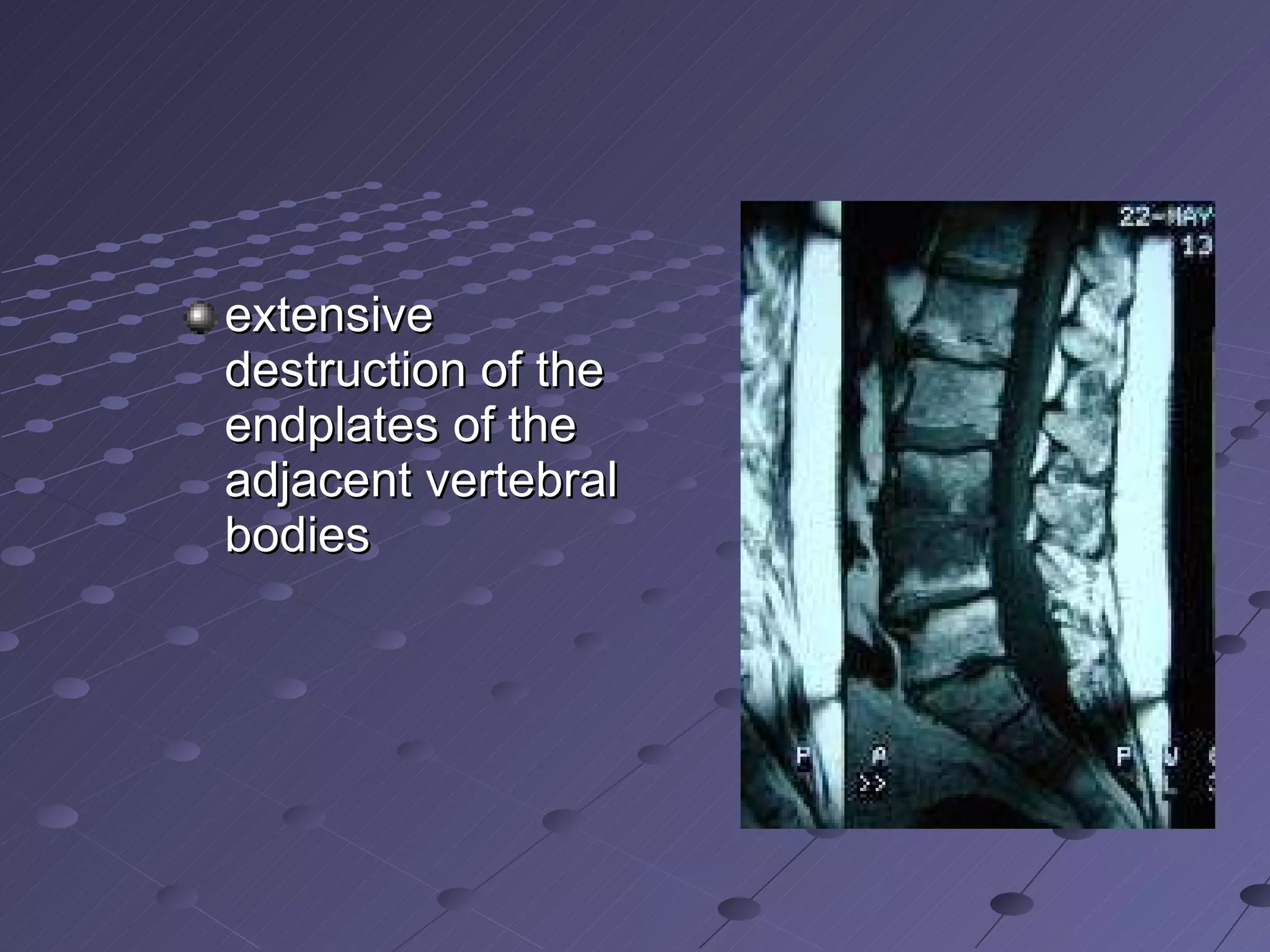
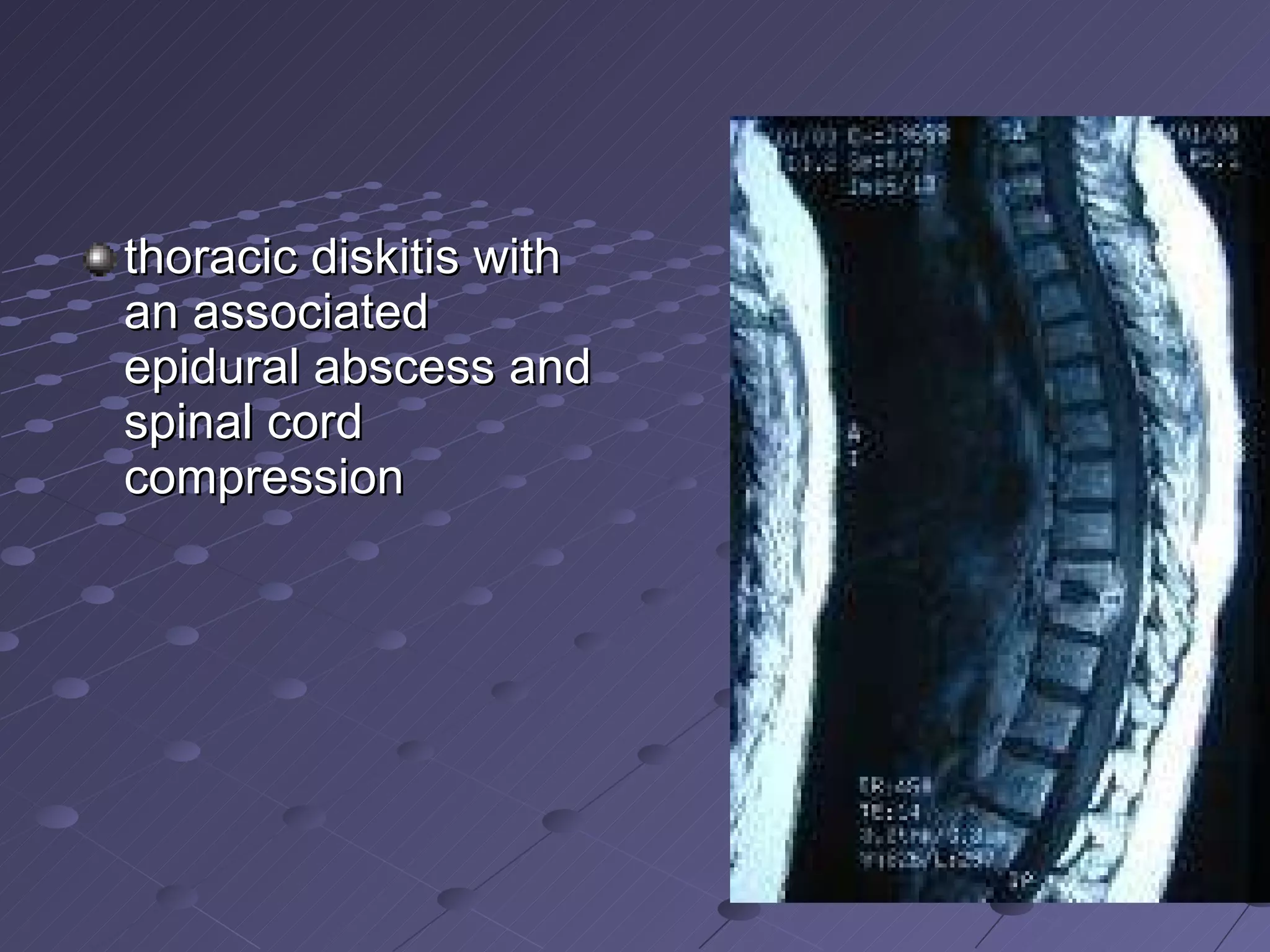
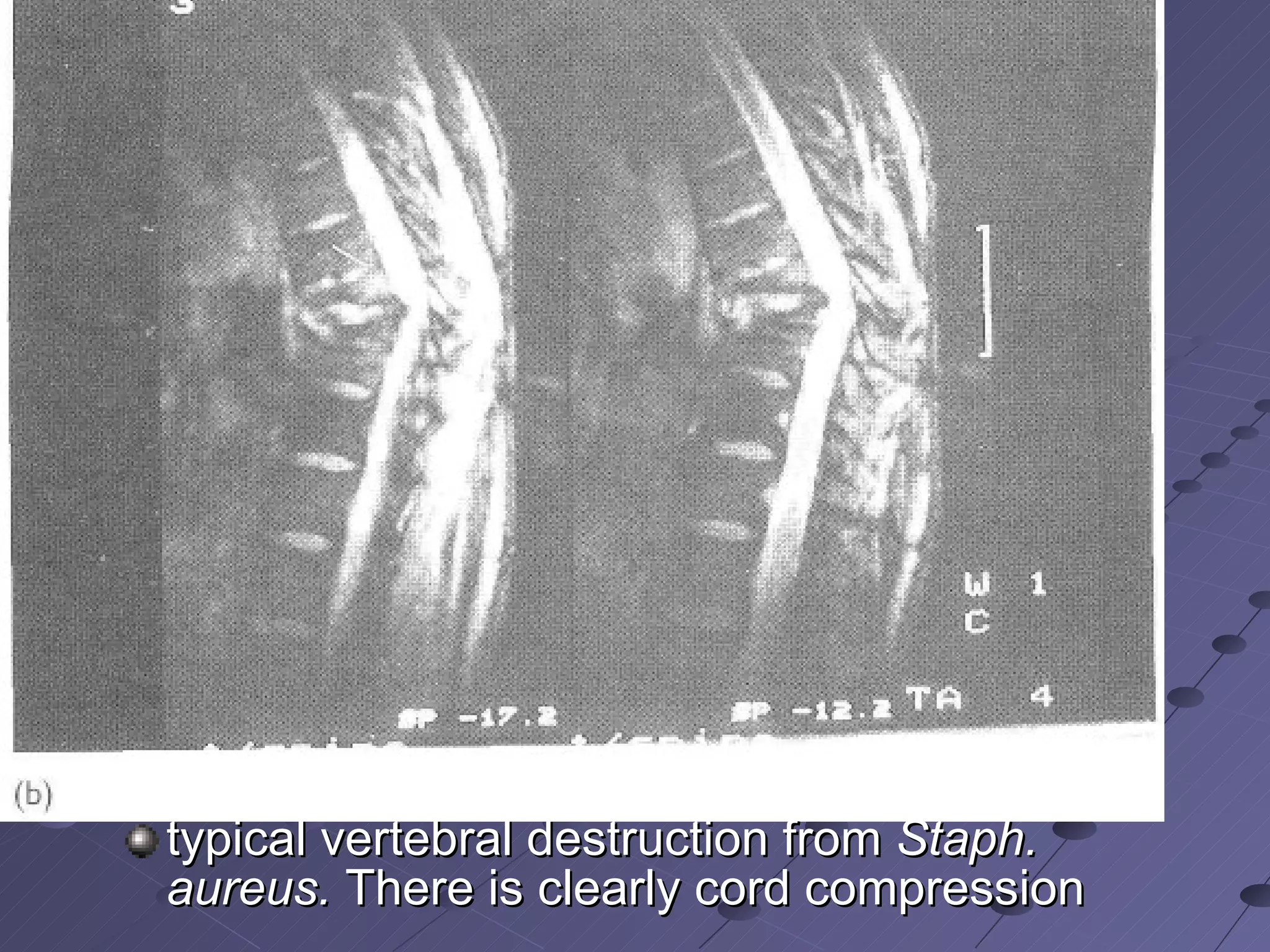
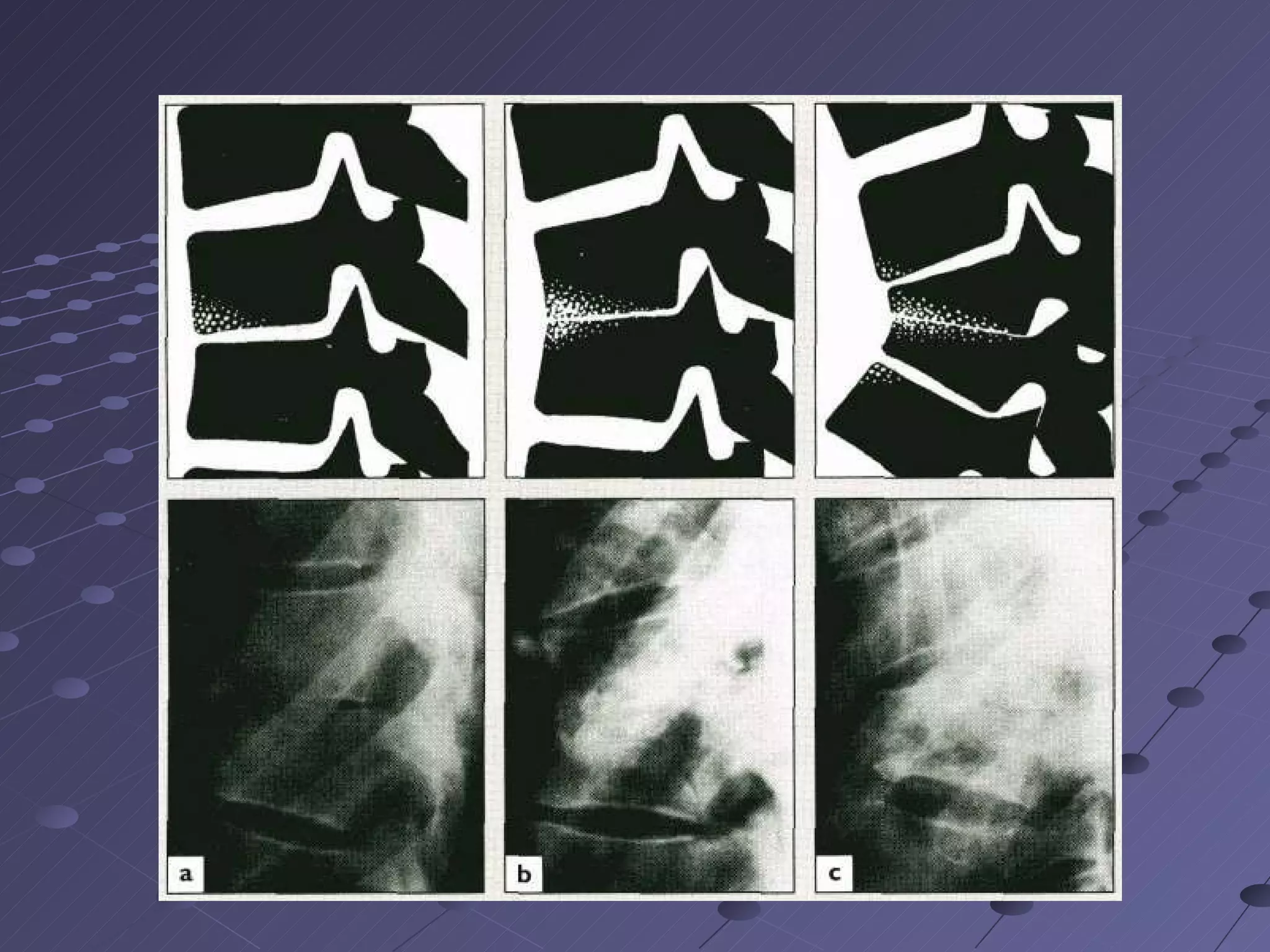
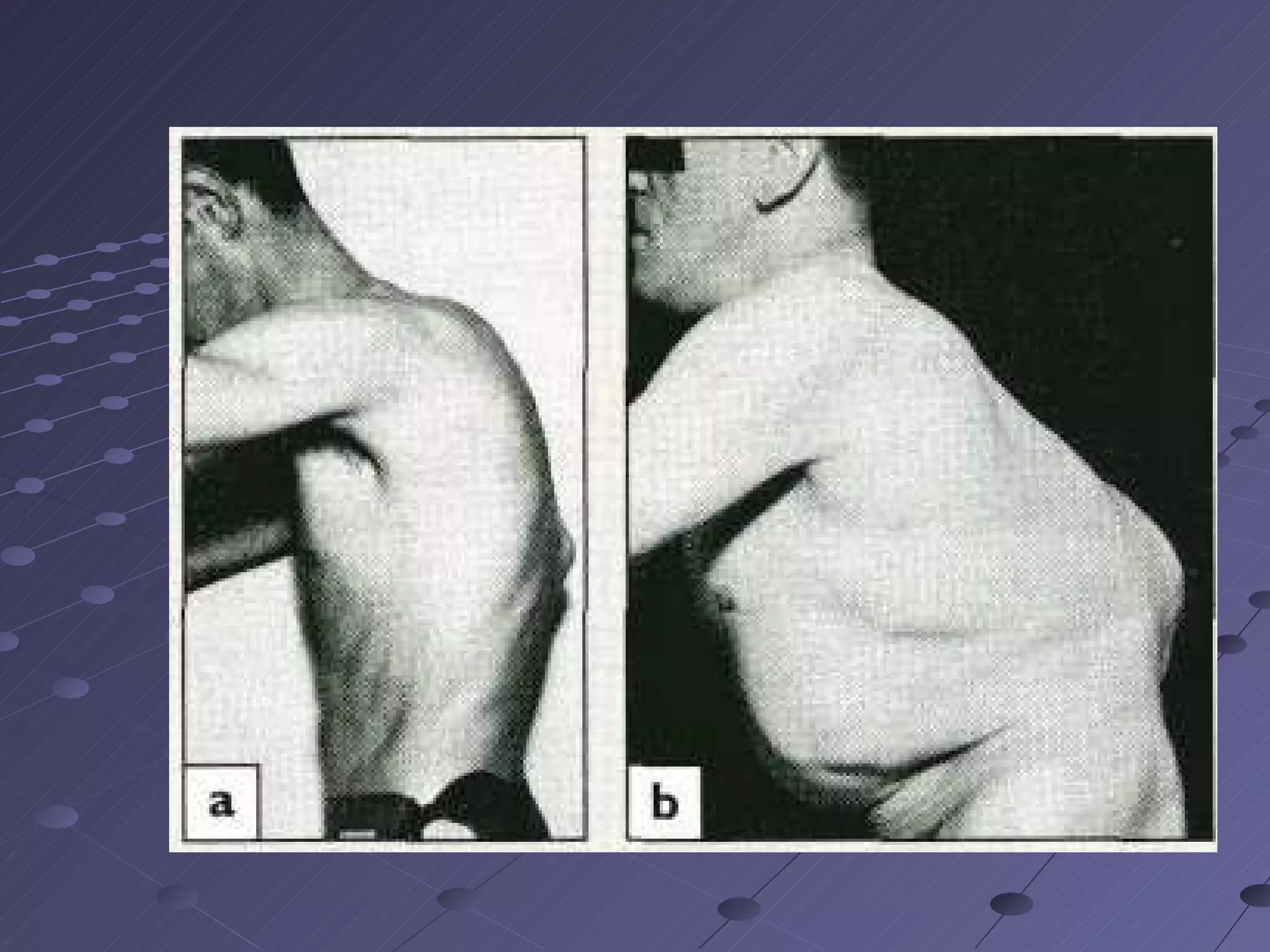
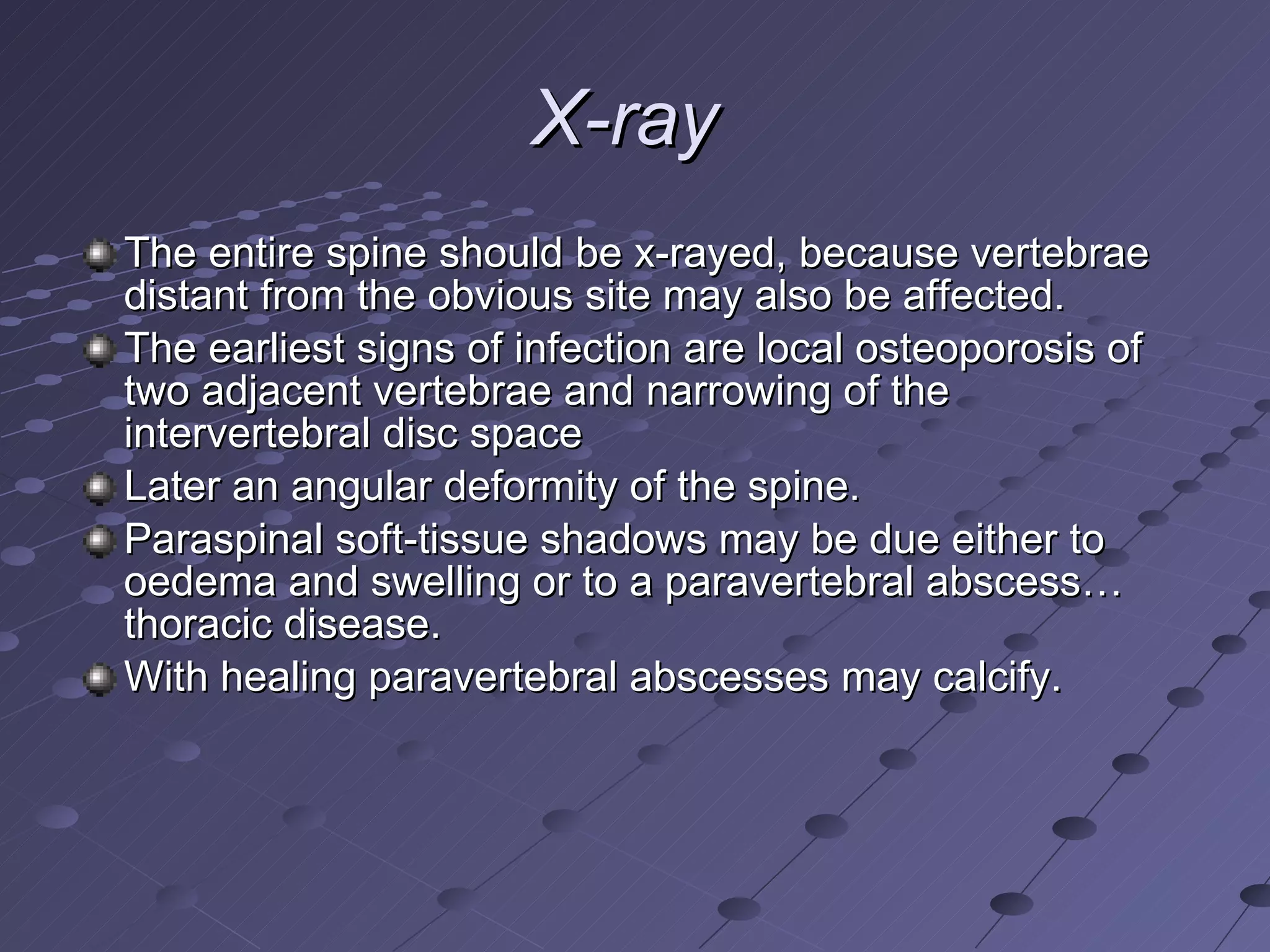
The document discusses different types of kyphosis (abnormal curvature of the spine), including congenital kyphosis, adolescent kyphosis, kyphosis in the elderly, and postural kyphosis. It covers the clinical features, investigations like x-rays and MRI, differential diagnoses, and treatment options for surgical and non-surgical management of kyphosis. Infections of the spine like tuberculosis are also discussed in terms of their pathology, clinical presentation, investigations, and treatment with antibiotics and surgery.