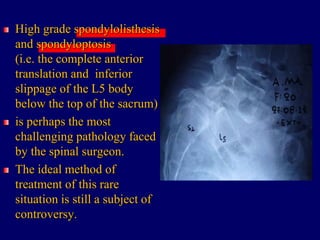
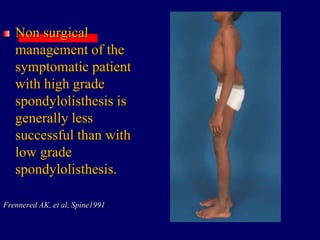
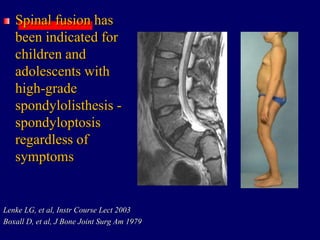
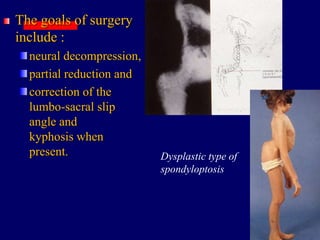
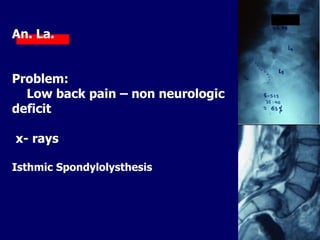
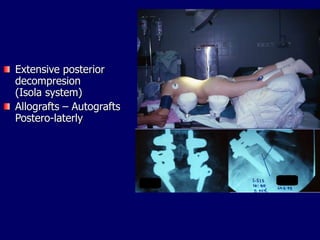
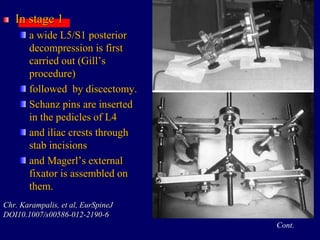
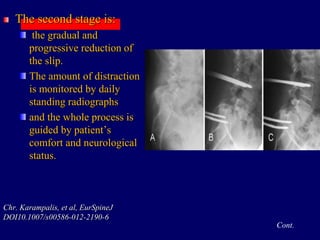
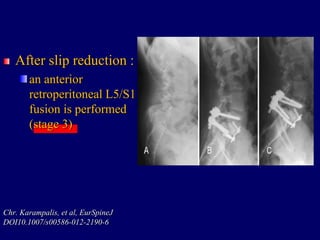
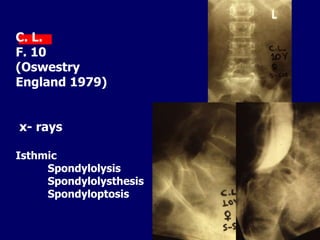
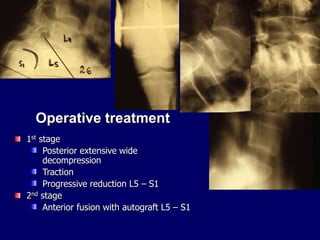
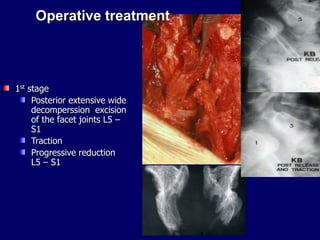
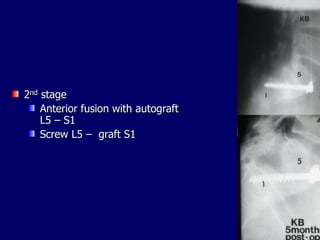
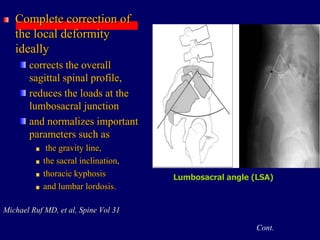
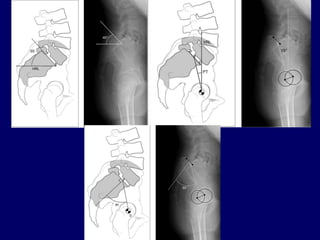
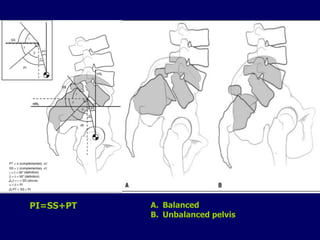
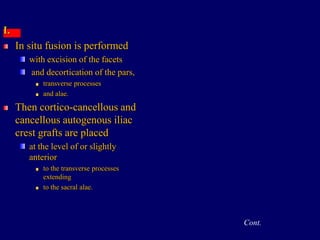
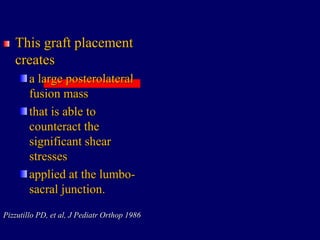
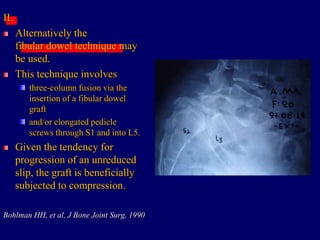
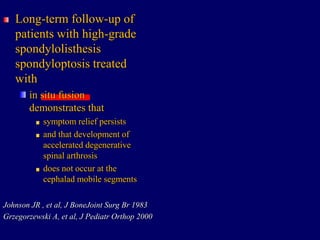
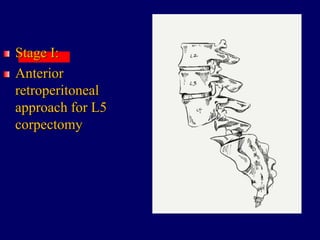
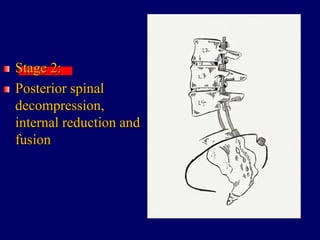
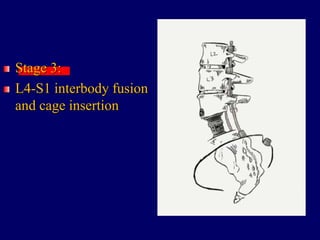
Spondyloptosis, or complete anterior translation of L5 below the sacrum, is a challenging pathology for spinal surgeons. There is no consensus on the ideal treatment. Surgical techniques proposed include complete or partial reduction with instrumentation and fusion, in situ fusion without reduction, and posterior osteotomies. The staged reduction method using external fixation described allows gradual reduction under assessment of neurological status to reduce risks. While reduction aims to restore alignment, it risks neurological injury, and in situ fusion is a safer alternative with similar outcomes when reduction is not necessary.