Acute otitis media final
- 1. ACUTE OTITIS MEDIA by DR.R.LATHIKA M.S(ENT PG) MODERATOR: Proff.Dr.DHINAKARAN M.S HOD DEPT OF ENT Scott Brown Learning 2020 Pediatrics- Volume II Chapter:14 Page no:137-152
- 2. INTRODUCTION • Common childhood infection • Hard to diagnose accurately • Acute otitis media (AOM) may be defined clinico pathologically as inflammation of the middle ear cleft of rapid onset and infective origin, associated with a middle ear effusion and a varied collection of clinical symptoms And signs.
- 3. • It normally develops behind an intact tympanic membrane but may include acute infections arising in the presence of ventilation tubes or existing tympanic membrane perforations
- 6. Subgroups of AOM • The literature supports four broadly defined subgroups of AOM: • 1. Sporadic: episodes occurring as infrequent isolated events, typically occurring with upper respiratory tract infections(URTIs) • 2.Resistant AOM: persistence of symptoms and signs of middle ear infection beyond 3–5 days of antibiotic treatment • 3. Persistent AOM: persistence or recurrence of symptoms and signs of AOM within 6 days of finishing a course of antibiotics • 4. Recurrent AOM: either 3 or more episodes of AOM occurring within a 6-month period, or at least 4–6 episodes within a 12- month period (no consensus has been reached on the latter).
- 7. • Grading of the severity of an episode has been attempted and has merit both clinically and for research. Pyrexia from 37.5 °C to 39 °C, vomiting and severity of otalgia have been used.
- 8. DIAGNOSIS • Diagnosis is based on the combination of often non- specific symptoms, evidence of inflammation of the middle ear cleft, and middle ear effusion • One third of children may have no ear-related symptoms. • Two-thirds may be apyrexial. • Symptoms suggestive of AOM include • rapid onset of otalgia, • hearing loss, • otorrhoea, • fever, • excessive crying
- 9. Symptoms (continued..) • irritability, • coryzal symptoms, • vomiting, • poor feeding, • ear pulling and clumsiness. • AOM most commonly develops 3–4 days after the onset of coryzal symptoms. • The otalgia will settle within 24 hours in two-thirds of • children without treatment. • The otorrhoea, if present, is mucopurulent and may be blood- stained. Symptomatic relief is obtained without treatment in 88% by day 4–7. • The hearing loss, caused by the middle ear effusion, • occurs early in the illness and may persist at greater than 20 dB for 1 month in over 30%, and 2 months in 20% of children.
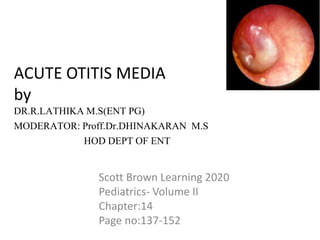
- 10. Signs • Diagnosis may be supported by otoscopic assessment of tympanic membrane colour, position and mobility. • In AOM the tympanic membrane is usually opaque. • It is most commonly yellow, or yellowish pink in colour, being red in only 18–19%. • The position of the tympanic membrane reliably predicts AOM only when it is bulging. • Hypomobility of the drum demonstrated by pneumatic otoscopy has been shown to aid diagnosis.
- 11. Investigations • Tympanometry may be used to establish the presence of a middle ear effusion but is not usually available. • Tympanocentesis and culture of middle ear effusion have been used in a number of studies assessing diagnostic. • It is rarely required to make the diagnosis, though may be considered in high-risk children: • such as the immunocompromised, • an unwell neonate, • those that fail to respond to conventional treatment, • &children who are seriously ill or have complications of AOM.
- 12. Investigations(continued..) • Taking a bacterial swab of persistent otorrhoea following perforation is recommended. • Nasopharyngeal swabbing for bacterial culture has been assessed but the correlation with has been too weak to recommend it clinically. • Both iron-deficiency anaemia and white blood cell disorders have been associated with AOM, so a full blood count is indicated. • Immunoglobulin assay may be appropriate: IgA, IgG (with subclasses) and IgM are typically assessed. • Children with recurrent infection of ventilation tubes may also merit investigation for primary ciliary dyskinesia, particularly - nasal and pulmonary symptoms coexist.
- 13. Differential diagnosis • Diagnostic confusion may occur with • acute mastoiditis, • OME, • otitis externa, • trauma, • Ramsay Hunt syndrome and bullous myringitis • Very rarely AOM may be the first indication of serious underlying disease such as Wegener’s granulomatosis or leukaemia.
- 14. Routes of spread of infection • Three potential routes are described: the Eustachian tube, tympanic membrane perforations or grommets, and haematogenous. • The Eustachian tube is traditionally assumed to be the main route by which organisms reach the middle ear. • negative middle ear pressure may facilitate • the movement of bacteria up the Eustachian tube. • similarities in organisms cultured from the postnasal space and the middle ear cleft in AOM.
- 15. Routes of spread of infection (CONTINUED..) • Altered tubal function may play a role. • Otitis-prone children have been shown to have • significantly poorer active tubal function (muscular opening function). • Pathogen entry through tympanic membrane perforations or ventilation tubes is most commonly associated with water exposure. • Haematogenous spread is provided by studies of viral identification in the blood and middle ear.
- 16. EPIDEMIOLOGY • AOM is one of the commonest illnesses of childhood • Incidences: • infants up to age 1 year- 60% • By age 3 years some 50–70% of all children will have had at least one episode of AOM, • By age 9 years-75%
- 17. • In the first 2 years of life AOM occurs bilaterally in 80% of cases. • After 6 years of age -unilateral in 86% • An important indicator of future problems is a first episode before 9 months of age- so,1 in 4 risk of developing recurrent AOM. • The incidence of AOM - varies with the seasonal incidence of viral upper respiratory infections
- 18. Risk factors • GENETIC FACTORS • IMMUNE FACTORS • ENVIRONMENTAL FACTORS • SYNDROMIC ASSOCIATIONS
- 19. GENETIC FACTORS • Certain HLA classes- significantly associated with increased risk of AOM. • Maternal blood group A is reported to an independent risk factor • A meta-analysis of risk factors has shown that, when one family member had had AOM, the risk increased for other family members • Racial differences are well described, with increases in American Indians, Inuits and Australian
- 20. IMMUNE FACTORS • A number of specific associations have been identified -defective or immature pathways may predispose to infection. • Low levels of IgG2 subclasses -more common in otitis-prone children. • Those with IgG2 deficiency were shown to be three times more likely to develop post-ventilation tube insertion otorrhoea, • for example-Delayed maturation of anti- pneumococcal antibodies (IgG1 and IgG2 were studied) does appear to predispose to AOM. • This may explain in part why children grow out of AOM as immunity matures.
- 21. IMMUNE FACTORS (CONTINUED..) Defective complement-dependent opsonization: low concentrations of mannose-binding protein which acts as an opsonin - a common defect with recurrent AOM and diarrhoea in infancy Aberrant expression of critical cytokines: Tumour necrosis factor and interleukins, resulting in suboptimal host defence, a cause for persistent infection. Expression of mucin genes: Middle ear mucosa expresses specifically the MUC5B gene. Mucin genes regulate the production of mucin.
- 22. IMMUNE FACTORS (CONTINUED..) • Children with HIV infection- Advanced disease associated with low CD4 counts-associated with an increased incidence of AOM. • Atopy has also been associated with increased risk of developing AOM.
- 23. ENVIRONMENTAL FACTORS • The most important is the children in the day-care attendance outside the home has greater the risk. • The incidence of AOM appears to follow : Seasonal URTIs in the winter months. Breastfeeding for 3 months is protective . Use of a pacifier (dummy) carries a relative risk(RR) of 1.45. Poor socioeconomic status poor housing overcrowding Passive smoke exposure from parental smoking The role of dietary factors=in particular cow’s milk allergy
- 24. Syndromic associations • Syndromes associated with abnormalities of skull base anatomy - associated with chronic middle ear disease. • Children with Turner syndrome do suffer more frequent episodes of AOM. • Down syndrome predisposes to middle ear disease including AOM. • CAUSES: • Cleft palate & Eustachian tube dysfunction • And increase in risk secondary to subtle immunological factors that predisposed to infection. • Children with primary ciliary dyskinesia if grommets are not inserted, or cystic fibrosis. • Iron-deficiency anaemia.
- 25. AETIOLOGY • Microbiological, anatomical and environmental factors combine with altered host defence mechanisms to predispose to infection. INFECTIVE AGENTS • AOM results from infection of the middle ear cleft. Both viral and bacterial infections, may occur in isolation or combination.
- 26. VIRUSES The viruses most commonly associated with AOM-in decreasing frequency include: RESPIRATORY SYNCYTIAL VIRUS (RSV), INFLUENZA A VIRUS, PARAINFLUENZA VIRUSES, HUMAN RHINOVIRUS ADENOVIRUSES
- 27. The viral material • Actively invade the middle ear cleft possibly by haematogenous spread • Some viruses may be actively invading the middle ear cleft, and may be contributing directly to mucosal inflammation. • Respiratory syncytial virus invaded the middle ear most frequently. • Passively invade along the Eustachian tube along with other nasopharyngeal secretions. • those arriving passively appear to cause AOM by virtue of their action on the Eustachian tube, on bacterial adherence and on host immunity.
- 28. VIRUSES (continued..,) • The ability of bacteria to colonize and adhere to the nasopharyngeal epithelium appears to be increased by certain viral infections. • Increased colonization by pathogenic bacteria may predispose to AOM • Viral and bacterial infections coexist in the middle ear cleft in AOM • Cell-mediated immunity has been affected by RSV infection • Neutrophil function altered by influenza viruses
- 29. BACTERIA • Streptococcus pneumoniae (pneumococcus) is the most common bacteria isolated from the middle ear in AOM, 18–55% of cases. There Are 90 serotypes. • Haemophilus influenza :16–37%, • Moraxella catarrhalis in 11–23% of cases. • Streptococcus pyogenes in up to 13% of cases • Staphylococcus aureus in up to 5%.
- 30. In the 1980s H. influenzae was the most common organism -Persistent or recurrent AOM, but this has been replaced by drug-resistant pneumococcus. After antibiotic treatment for recurrent AOM it is now estimated that 50% of H. influenzae are beta-lactamase producing. Penicillin resistance in pneumococci results from decreased penicillin-binding protein on the bacterial cell walls so reducing the affinity for penicillin-related drugs, but resistance may often be overcome by increasing drug dosage.
- 31. • Most M. catarrhalis are now beta-lactamase producing. • Studies on HIV-positive children suggest a similar spectrum • severely immunosuppressed higher percentage of Staphylococcus aureus has been reported.
- 32. Management of acute episodes • CONSERVATIVE TREATMENT • Most children will benefit from simple analgesics and antipyrexials. • Paracetamol and ibuprofen are most commonly used. • ibuprofen provides additional benefit by reducing mucosal inflammation when taken in combination with amoxicillin
- 33. CONSERVATIVE TREATMENT • Antibiotics • Antihistamines and decongestants • Xylitol • Zinc • Vaccination • Benign commensals • Immunoglobulins •
- 34. Antibiotics • Amoxicillin remains the first choice in most centres higher than previously recommended doses (80 mg/kg/day) if drug-resistant pneumococci are common in a particular country or region, • With macrolides for penicillin-sensitive patients. • For persistent or resistant episodes, depending on the prevalence of beta-lactamase producing organisms, and culture results if available. • Options include amoxicillin-clavulanate or cefuroxime axetil orally, or intramuscular ceftriaxone
- 35. Antihistamines and decongestants • the use of oral or intranasal antihistamines and/or decongestants concluded that their use reduce persistent AOM at 2 weeks Xylitol Xylitol is a commonly used sweetener that inhibits pneumococcal growth and the attachment of pneumococcia nd Haemophilus to nasopharyngeal cells. As such, it is a recognized prophylaxis for AOM when administered via chewing gum or syrup.
- 36. Zinc • Zinc is a micronutrient found in a variety of foods and is essential for immune function and resistance to infection. • Beneficial effect in the prevention and treatment of pneumonia and other respiratory conditions. Vaccination • Vaccines have been used effectively against most common childhood infections caused by single specific organisms such as mumps, measles and rubella. • Potential obstacles include the wide range of causative organisms, both bacterial and viral, the varied serotypes. • Influenza A vaccination is currently the only commercially available preparation for the prophylaxis of viral upper respiratory tract infections • immunization against Haemophilus influenzae type b (Hib) was introduced.
- 37. SURGICAL PROPHYLAXIS 1. Ventilation tubes: decrease in episodes of AOM of 56%. • COMPLICATIONS: a higher incidence of tympanosclerosis and focal areas of tympanic membrane atrophy 2. Adenoidectomy and adenotonsillectomy: • Adenoidectomy considered in those children who have failed medical therapy and • AOM following ventilation tube insertion. • The presence of OME increases the benefit of adenoidectomy.
- 38. OUTCOMES An episode of AOM may: • resolve rapidly with or without antibiotics • prove resistant to first-line antibiotics • persist or recur shortly after a course of antibiotics has finished • subsequently recur progress to tympanic membrane perforation or other complication of infection.
- 39. Outcomes MIDDLE EAR EFFUSIONS Middle ear effusions are an important outcome of AOM. AUDITORY FUNCTIONING 1 in 3 children will have an air– bone gap greater than 20 dB at 1 month after infection, and 1 in 5 at 3 months. SPEECH AND LANGUAGE DEVELOPMENT different cognitive development in school-age children with a history of otitis media in the first 3 years of life. Occur in the early years of life on expressive language development but not receptive language.
- 40. COMPLICATIONS
- 41. COMPLICATIONS Extracranial complications TYMPANIC MEMBRANE PERFORATION • Tympanic membrane perforation is considered a complication of AOM. It is the commonest complication of infection and is reported in 0–10% of episodes. • Perforation is associated with a purulent or bloody otorrhoea and immediate relief of pain. • It typically occurs in the posterior half of the pars tensa, and is associated with loss of the fibrous middle layer of the drum. • This may predispose to future posterior retraction pockets. Four outcomes of perforation may result: 1. In most cases the perforation heals spontaneously and the infection resolves. 2. The infection may resolve but the perforation may persist. 3. This may predispose the ear to future AOM or chronic suppurative otitis media. 4. The perforation and otorrhoea may persist, manifesting as chronic suppurative otitis media. ‘Chronicity’ is generally deemed to have occurred by 3 months.
- 42. • Haemophilus influenzae is the dominant otopathogen cultured in AOM with tympanic membrane perforation (followed by streptococcus pneumoniae, then moraxella catarrhalisweeks). • The location and size of the perforation correlates to the resulting degree of sound conduction impairment. • With larger perforations and those located in the anteroinferior quadrant leading to a larger conductive deficit.
- 44. ACUTE MASTOIDITIS • Four classes of mastoiditis are defined. During episodes of acute otitis media infection and inflammation may naturally extend into the mastoid cavity and be visualized radiologically. • This is not associated with the typical signs of acute mastoiditis and is not considered a complication of AOM. • Infection may spread to the mastoid periosteum by emissary veins: acute mastoiditis with periosteitis. • At this stage no abscess is present but the postauricular crease may be full, the pinna may be pushed forward, and there may be mild swelling, erythema and tenderness of the postaural region.
- 46. ACUTE MASTOIDITIS (continued..,) • When acute mastoid osteitis develops, the infection has begun to destroy the bone of the mastoid air cells, and a subperiosteal abscess may develop. • Signs may be similar to those when periosteitis is present. • A subperiosteal abscess develops most commonly in the postauricular region. • A zygomatic abscess may develop above and in front of the pinna • . A Bezold abscess may result from perforation of the medial mastoid cortex, tracking down sternomastoid to the posterior triangle.
- 47. ACUTE MASTOIDITIS (continued..,) • Pus tracking down peritubal cells may result in a retropharyngeal or parapharyngeal abscess. • A fourth stage may be reached, subacute (‘masked’) mastoiditis, • in incompletely treated AOM after 10–14 days of • infection. Signs may be absent but otalgia and fever persist. • This stage can also progress to serious complications.
- 48. ACUTE MASTOIDITIS Symptoms • Otalgia and irritability in most children. • Diagnosis: • Postauricular swelling in 80–95% of cases, • Protrusionof the pinna in 95–100%. • Postauricular erythema and tenderness over macewen’s triangle (on palpation through the conchal bowl). • Pyrexia in 81%. • Otorrhoea in 30%. • Clinically, a red or bulging tympanic membrane will often be seen. • A normal drum does not exclude the diagnosis,it result from resolution of the mesotympanic infection following antibiotic treatment while the osteitis in the mastoid progresses. • Sagging of the posterior wall of the external auditory canal, resulting from subperiosteal abscess formation
- 49. ACUTE MASTOIDITIS Pathogens • Streptococcus pneumoniae, • Streptococcus pyogenes, • Pseudomonas aeruginosa • Staphylococcus aureus are the most commonly • reported in order of decreasing frequency. • Haemophilus influenzae • Moraxella catarrhalis, • Proteus mirabilis and Gram-negative anaerobes • Fusobacterium necrophorum
- 50. • Clinical features may vary in accordance with the pathogen isolated. • Streptococcus pneumoniae appears to lead to more severe symptoms and a higher incidence of mastoidectomy. • S. pyogenes causes less otalgia. • Pseudomonas aeruginosa particularly affects children with ventilation tubes
- 51. • A full blood count, CRP and blood cultures are often obtained. • A CT scan of the mastoid is recommended: 1. When intracranial complications are present or suspected (though MRI may be more helpful in identifying specific intracranial pathology), 2. When mastoidectomy is to be performed, 3. Those not improving on antibiotic treatment. • A CT scan may show evidence of osteitis, abscesses and intracranial complications.
- 52. • Although simple mastoidectomy represents the most reliable and effective surgical method to treat acute mastoiditis, a more conservative approach consisting of adequate parenteral antibiotic coverage with or without myringotomy is being increasingly adopted for children suffering from uncomplicated acute mastoiditis. • The antibiotic of choice is third-generation cephalosporin, or an aminopenicillin combined with a β-lactamase inhibitor. • If Pseudomonas aeruginosa is suspected, treatment includes ciprofloxacin, piperacillin or fosfomycin.
- 53. Differential diagnosis • INCLUDES 1. AOM, 2. Otitis externa, 3. Furunculosis and reactive lymphadenopathy. 4. Rarely, undiagnosed cholesteatoma, 5. Wegener’s granulomatosis, 6. Leukaemia and histiocytosis may first present with aom, hence tissue should be sent for histology if mastoidectomy is performed
- 54. • If there is a suspicion of intracranial complication and those not responding to conservative treatment should undergo cortical mastoidectomy. • This may be combined with myringotomy with or without ventilation tube placement, and culture of the aspirate. • This can be challenging surgery for the less experienced as the mastoid is often full of granulations and the facial nerve superficial in the young child. • the appropriate duration of observation prior to proceedings 24–72 hours. • The presence of a subperiosteal abscess, an unwell child,or a deteriorating clinical picture should prompt more rapid intervention.
- 55. PETROSITIS • Infection may extend to the petrous apex. • The classic features of Gradenigo’s triad 1. VI nerve palsy, 2. severe pain in the trigeminal nerve distribution 3. middle ear infection • Decompression of the petrous apex. • Resolution of the sixth nerve palsy from almost instant recovery to upto 6 weeks. • Many patients -successfully managed conservatively with administration of parenteral antibiotics, and • Reserve surgery for those not responding to conservative management. • Sixth nerve palsy resolution with conservative treatment can take up to 3 months.
- 57. LABYRINTHITIS • Round window permeability changes during acute infection are important as these may allow entry of bacterial toxins. • Permeability can be increased by streptococcal toxins. • Preformed channels for bacterial entry may also exist, such as surgical or congenital perilymph fistulae. • These may allow infection to spread directly to the subarachnoid space causing meningitis. • Particular concern arises in children with congenital inner ear abnormalities, and those with cochlear implants. • Three types of labyrinthitis are recognized. • Perilabyrinthitis is not associated with aom. • Serous labyrinthitis is inflammation of the labyrinth without pus formation, characterized by • Sensorineural hearing loss and vertigo, usually in a non-toxic patient. • There may be an additional conductive loss secondary to the presence of fluid. • Typically there is complete and rapid recovery of auditory and vestibular function.
- 58. Suppurative labyrinthitis May result from spread of infection from the mastoid or middle ear May raise the suspicion of an anatomical defect or immune deficiency. Severe vertigo, nausea, vomiting, nystagmus and permanent hearing loss The nystagmus exhibit various patterns-due to differential effects on inner ear function by toxic or inflammatory mediators, direction-fixed, irritative-type is the most common observed pattern Suppurative labyrinthitis is rare, and diagnosis is usually made based on clinical and audiometric findings.
- 59. Suppurative labyrinthitis • MRI, if performed, may demonstrate contrast enhancement of the labyrinth and there is • some evidence to suggest the degree of enhancement . • CT is not helpful in diagnosis but may help to delineate underlying anatomical abnormalities.53 • The treatment of cases ranges from ventilation tube insertion and aggressive antibiotic use, to tympanomastoidectomy and cochleotomy. • Resolution of the vertigo may take weeks to months to occur, demonstrating contralateral vestibular system compensation,rather than recovery of function of the affected ear. • Longer-term complications of suppurative labyrinthitis may include labyrinthitis ossificans, caused by fibrous or bony replacement of the labyrinth. • The administration of steroids during the initial phase of the illness may help
- 60. Intracranial complications • MENINGITIS • EXTRADURAL ABSCESS • SUBDURAL EMPYEMA • SIGMOID SINUS THROMBOSIS • CEREBRITIS, • BRAIN ABSCESS AND • OTITIC HYDROCEPHALUS.
- 61. Intracranial complications • The most common symptoms associated with an intracranial complication include • fever, otalgia, cephalgia and • reduced general condition, • altered mental status
- 62. MENINGITIS • Meningitis is usually cited as the commonest intracranial complication of AOM, accounting for 54–91% of cases. • The earliest symptoms are headache, fever, vomiting, photophobia, irritability and restlessness, with fullness of the anterior fontanelle in children under 22 months of age. • Diagnosis is usually made on the clinical presentation, with a lumbar puncture demonstrating white blood cells and low glucose in the CSF. • Younger children, average age 2 years, are most commonly infected. • The rate of Haemophilus influenzae type b meningitis has dropped dramatically since vaccination was introduced. • Streptococcus pneumoniae is the causal agent in a greater proportion because of this reduction.
- 63. MENINGITIS • Treatment is medical and should comprise a third generation cephalosporin with consideration given to the addition of vancomycin to cover for resistant strains. • Addition of dexamethasone may reduce • potential neurological sequelae, although have no effect on audiological outcome. • If mastoid surgery is required, it is usual to wait for an improvement in the medical condition of the child first if possible.
- 64. EXTRADURAL ABSCESS • This is the next commonest intracranial complication. • It is more commonly associated with chronic disease. • Pus collects between dura and bone, usually after bone erosion. • If this lies in the posterior fossa medial to the sigmoid sinus, it is termed an extradural (epidural) abscess; • if it is within the split of dura enclosing the sigmoid sinus, it is called a perisinus abscess. It may be discovered only at mastoidectomy, may be suspected in the patient with • persistent headache and fever, or severe otalgia. • Treatment is surgical drainage.
- 66. SIGMOID SINUS THROMBOSIS • Incidence of 0–2.7% • M/c : results from erosion of the bone over the sinus from mastoiditis, and may also be associated with other complications. • It occurs in association with otitis media alone in 43% of cases. • Infected thrombus develops within the sinus and may then extend proximally and distally to the internal jugular vein and superior vena cava, entering the systemic circulation and causing septicaemia. • In addition to mri is the imaging of choice showing an acute clot as isodense on t1 and hypodense on t2, with a subacute clot becoming hyperintense on t1.
- 67. • headache and otorrhoea, a spiking pyrexia may develop. • Griesinger’s sign is mastoid tenderness and oedema secondary to thrombophlebitis of the mastoid emmisary vein. • The presence of specific neurological signs and symptoms is significantly correlated with hypoplasia of the contralateral venous sinus • The presence of Fusobacterium necrophorum dictates a more aggressive and prolonged clinical course.
- 69. • The addition of MR venography will demonstrate lack of flow and increase the sensitivity of the diagnosis especially in the early stage. • Management options include the use of systemic broad-spectrum antimicrobials. • Non-pneumococcal streptococcal, anaerobic and staphylococcal species are commonly implicated and therefore ceftriaxone, metronidazole or clindamycin are commonly used
- 70. The surgical approach • Myringotomy with ventilation tube placement, • Mastoidectomy with or without delamination of the sigmoid sinus, • Needling of the sinus or thrombectomy. • Internal jugular vein ligation and craniotomy • use of post-operative anticoagulation also varies between institutions, with duration ranging from 6 weeks to 6 months.
- 71. OTITIC HYDROCEPHALUS • This is a complication of AOM manifesting as raised intracranial pressure in the absence of any space-occupying lesion, and without obstruction to the flow of CSF. • Benign intracranial hypertension is a synonym. • The aetiology is obscure. • Headache is the predominant symptom. • Associated with drowsiness, vomiting, visual disturbance and diplopia, with signs of papilloedema and abducens nerve palsy on examination. • It is commonly associated with sigmoid or transverse sinus thrombosis • MRI/MRV are important investigations. • Lumbar puncture will show raised CSF pressure, but normal CSF composition. • medical treatments may be tried such as corticosteroids, mannitol, diuretics and acetazolamide
- 72. FOCAL OTITIC ENCEPHALITIS (CEREBRITIS) • Focal inflammation and oedema of brain tissue may occur independent of or in association with any suppurative complication of AOM. • Intensive antibiotic treatment is required.
- 73. Brain abscesses • Brain abscesses are more commonly associated with chronic ear disease but may occur in association with • AOM and its complications. • They form a larger proportion of complications in developing countries. • They develop in both the temporal lobe and cerebellum. In the setting of acute mastoiditis, the most common causative organism is • S. pneumoniae or other non-pneumococcal Streptococcus sps
- 75. • Persistent headaches are the commonest symptom. • Initial symptoms may be of encephalitis, but these often settle as the abscess organizes over days or weeks. • Eventually, signs of raised intracranial pressure, focal neurology and infection develop. Investigations include CT imaging followed by lumbar puncture if safe. • Patients should undergo treatment with broad- spectrum antibiotics and mastoidectomy to remove the infective foci. In the early stages of cerebritis neurosurgical drainage may be avoided, but it will be required if the abscesses are expanding. • Brain abscesses carry a potentially high mortality rate, causes. • The presence of morbidity such as sensorineural hearing loss, vestibular dysfunction and neurologicalsequelae variesfrom 20% to 79%
