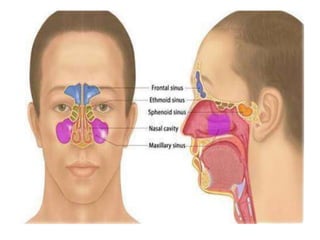
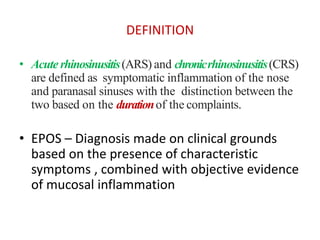
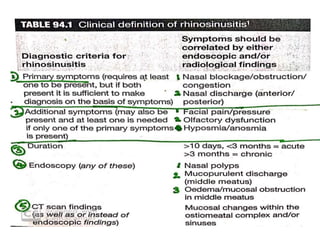
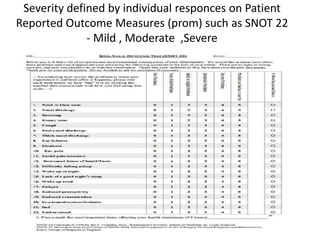
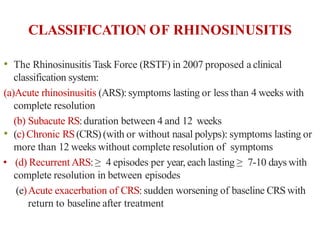
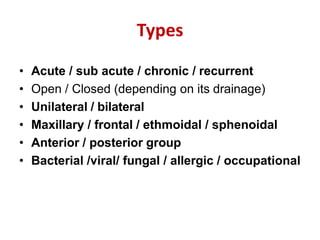
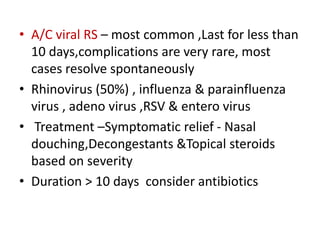
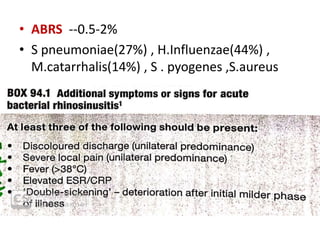
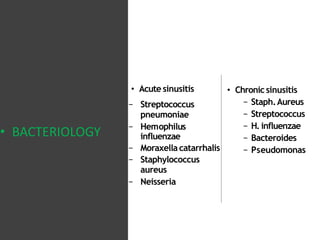
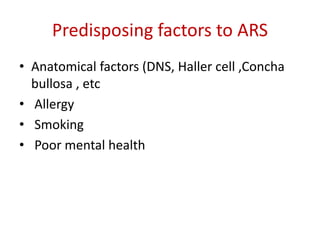
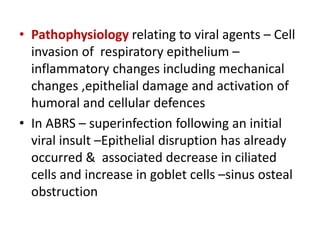
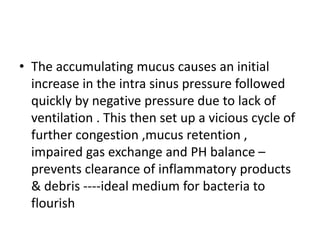
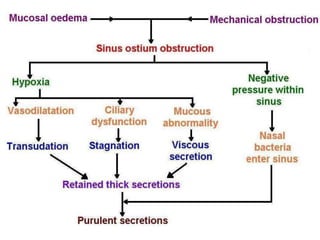
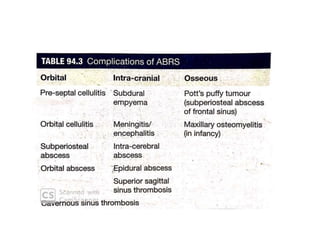
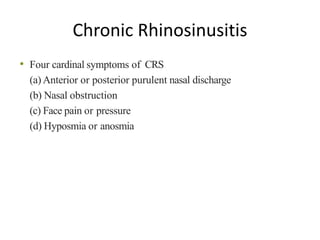
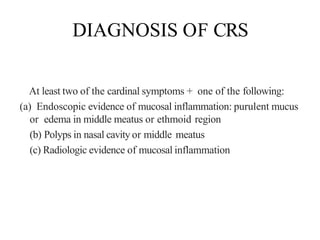
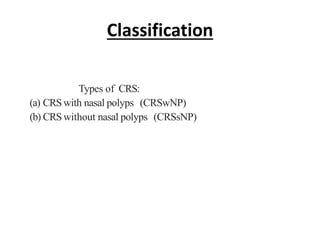
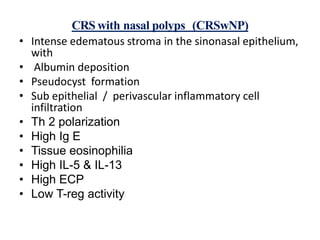
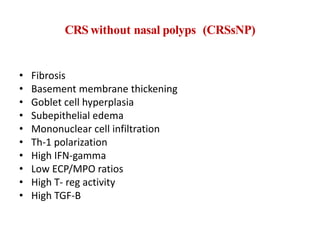
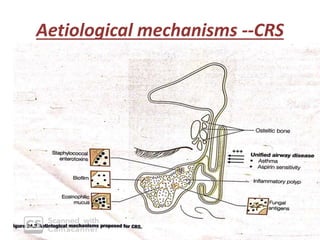
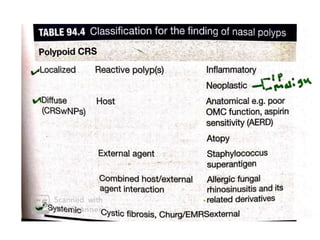
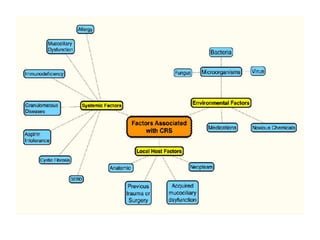
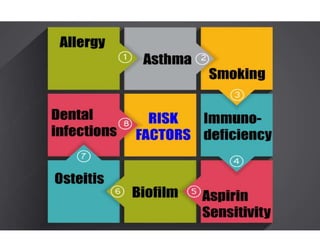
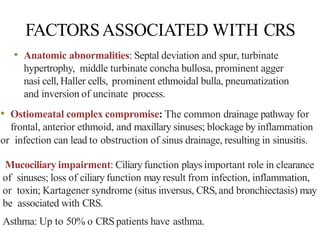
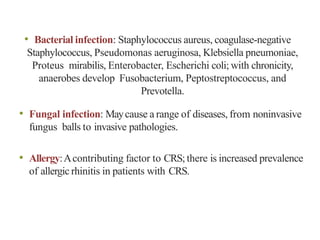
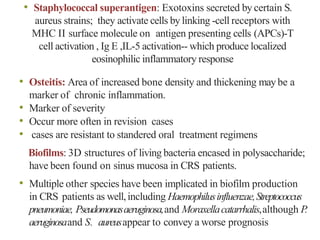
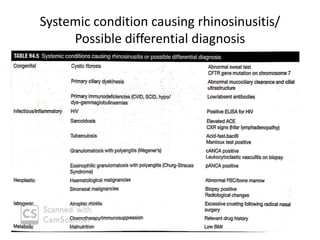
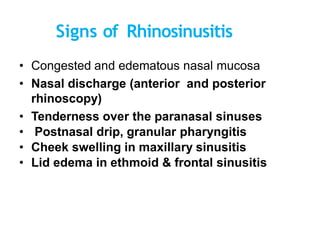
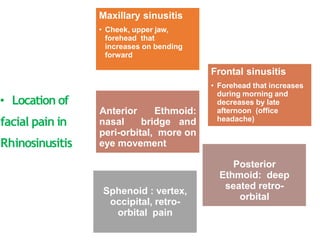
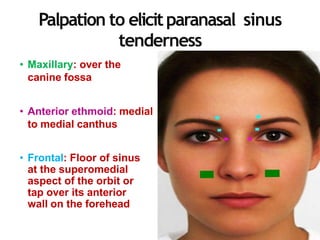
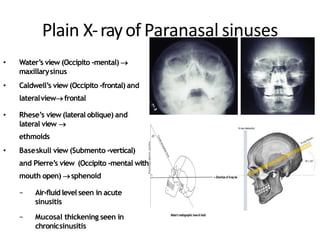
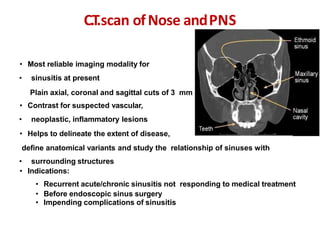
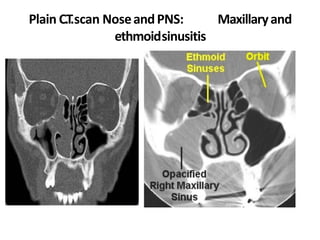
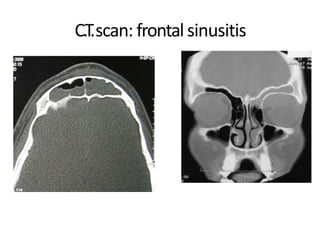
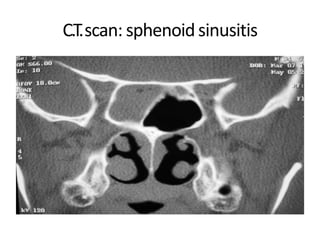
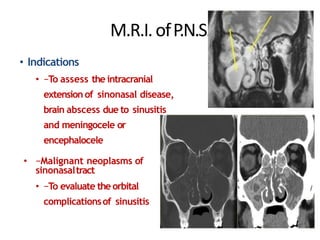
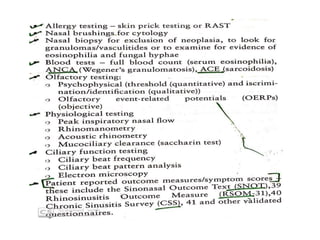
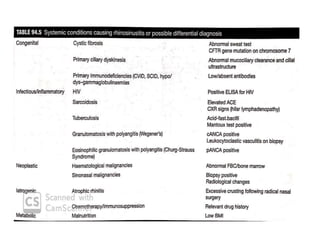
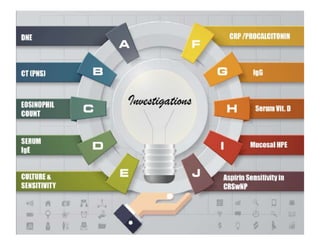
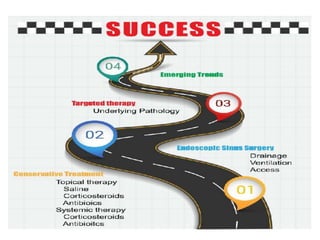
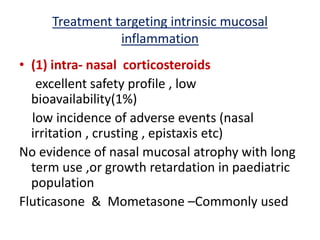
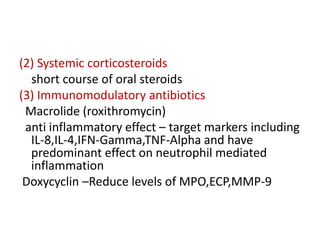
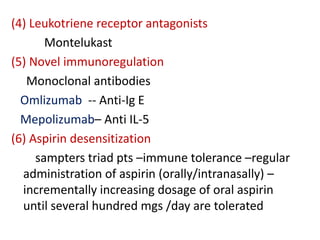
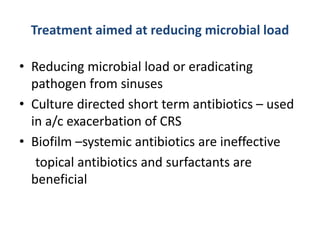
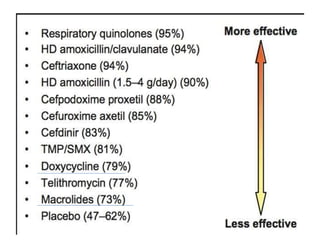
This document provides information about rhinosinusitis, including definitions, classifications, signs, symptoms, investigations and treatment. It defines acute and chronic rhinosinusitis based on duration of symptoms. Common causes include viral and bacterial infections. Chronic rhinosinusitis is classified as with or without nasal polyps. Diagnosis involves symptoms and endoscopy or CT scan findings. Treatment aims to reduce inflammation, bacterial load and improve mucociliary clearance using medications, sinus irrigation and surgery.