The document provides a comprehensive overview of otitis media, including its definition, epidemiology, clinical manifestations, and management strategies for a 6-year-old male patient diagnosed with the condition. It outlines patient demographics, relevant history, and investigative procedures, such as otoscopic examination and tympanometry. Management recommendations emphasize the use of amoxicillin as the first-line treatment to address the primary pathogens involved.




![6 | P a g e
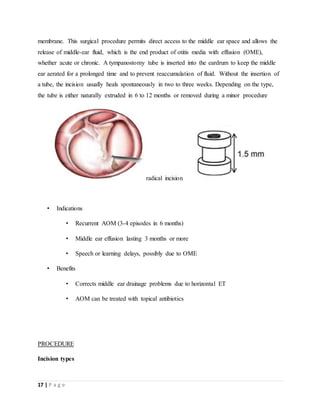
Otitis media with effusion (OME), also known as serous otitis media (SOM) or secretory
otitis media (SOM), and colloquially referred to as 'glue ear,'[25] is fluid accumulation
that can occur in the middle ear and mastoid air cells due to negative pressure produced
by dysfunction of the Eustachian tube. This can be associated with a viral URI or
bacterial infection such as otitis media (Rosenfeld RM., 2004).
Chronic suppurative OM
Chronic suppurative otitis media (CSOM) is a chronic inflammation of the middle ear
and mastoid cavity that is characterized by discharge from the middle ear through a
perforated tympanic membrane for at least 6 weeks
Adhesive OM
Adhesive otitis media occurs when a thin retracted ear drum becomes sucked into the
middle-ear space and stuck (i.e., adherent) to the ossicles and other bones of the middle
ear.
Epidemiology
Acute otitis media is very common in childhood. It is the most common condition for which
medical care is provided in children under five years of age in the US (John D.D., 2013). Acute
otitis media affects 11% of people each year (709 million cases) with half occurring in those
below five years (Monasta L.,2012) Chronic suppurative otitis media affects about 5% or 31
million of these cases with 22.6% of cases occurring annually under the age of five years. Otitis
media resulted in 2,400 deaths in 2013—down from 4,900 deaths in 1990(GBD.,2013).
Predisposing factor
The risk factors for OM include:
being between 6 and 36 months old
using a pacifier
attending daycare
being bottle fed instead of breastfed (in infants)
drinking while laying down (in infants)
being exposed to cigarette smoke](https://image.slidesharecdn.com/otitismedia-190809143438/85/OTITIS-MEDIA-CASE-PRESENTATION-CASE-STUDY-6-320.jpg)

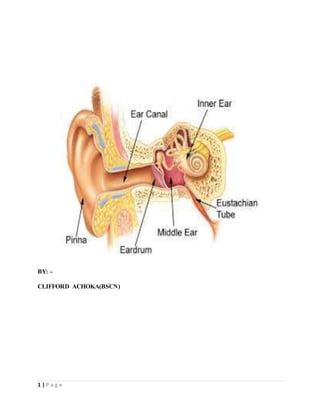
![8 | P a g e
2. Stage of exudation: Exudate collects in the middle ear and ear drum is pushed laterally.
Initially the exudate is mucoid, later it becomes purulent.
3. Stage of suppuration: Pus in the middle ear collects under tension, stretches the drum &
perforates it by pressure necrosis & the exudate starts escaping into external auditory canal.
4. Stage of healing: The infection starts resolving from any of the stages mentioned & usually
clears up completely without leaving any sequelae.
5. Stage of complications: Infection may spread to the mastoid antrum. Initially it causes
Catarrhal mastoiditis [congestion of the mastoid mucosa], stage of Coalescent mastoiditis &
later empyema of the mastoid.
Clinical manifestation
1. Catarrhal stage (stage of congestion)
Fullness or heaviness in the ear
Severe ear pain at night
Deafness
Tinnitus (ringing or buzzing in the ear)
Autophony (spoken words of patient echo in his
ears)
TM (ear drum) gets retracted
Cart wheel appearance of ear drum
Absence of light reflex
2. Stage of exudation
All symptoms become more severe.
3. Stage of suppuration
Perforation of Ear drum
Otorrhoea with mucoid purulent discharge
Pulsatile discharge (ear discharge with each arterial dilation) [Lighthouse sign]
4. Stage of healing](https://image.slidesharecdn.com/otitismedia-190809143438/85/OTITIS-MEDIA-CASE-PRESENTATION-CASE-STUDY-8-320.jpg)