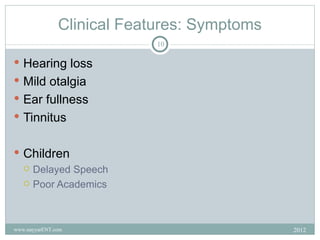
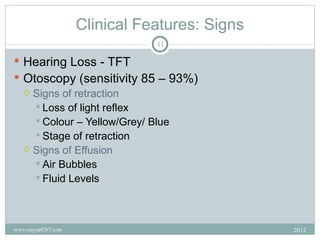
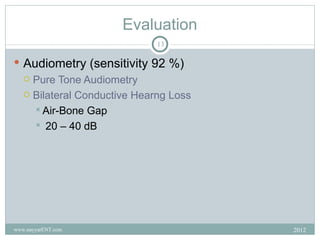
1) Otitis media with effusion (OME), also known as glue ear, is a chronic accumulation of fluid in the middle ear behind an intact but retracted eardrum that can cause hearing loss.
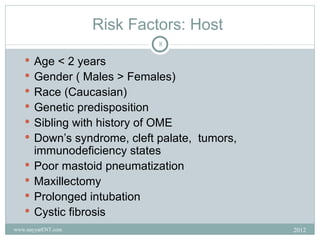
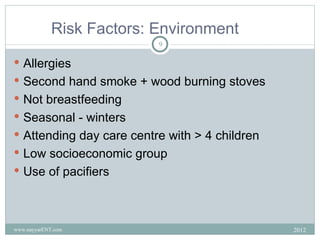
2) It commonly affects young children, with the highest prevalence between ages 2-5 years old. Risk factors include age, male gender, family history, and exposure to smoke.
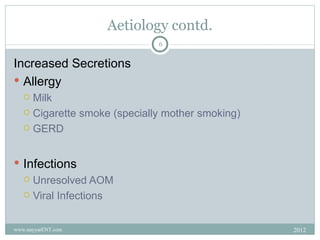
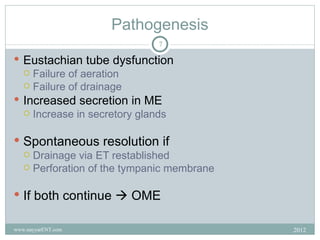
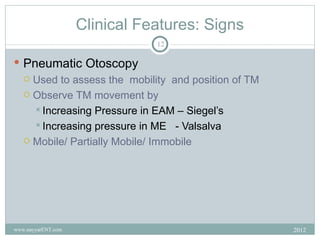
3) The fluid is caused by eustachian tube dysfunction preventing drainage and ventilation of the middle ear, which can be due to infections, allergies, or adenoid hypertrophy among other factors.