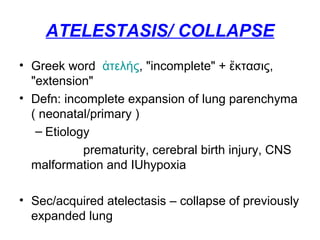
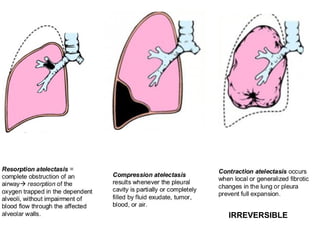
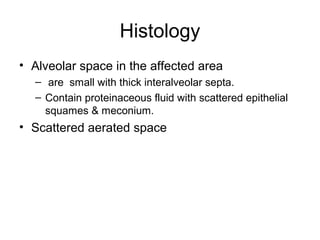
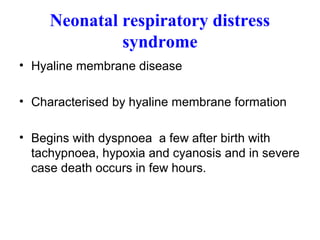
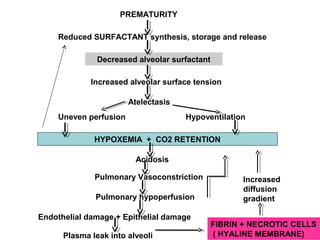
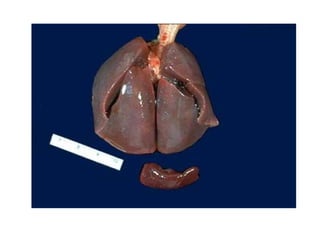
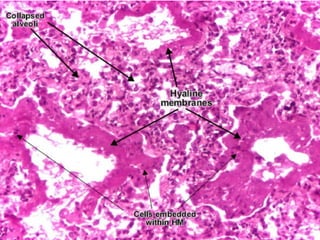
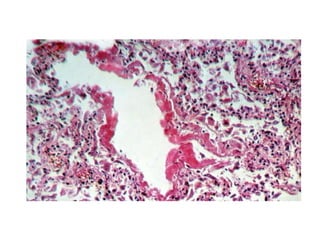
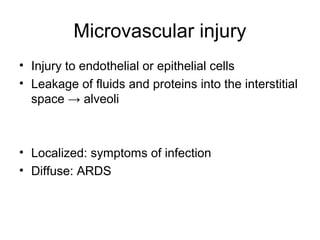
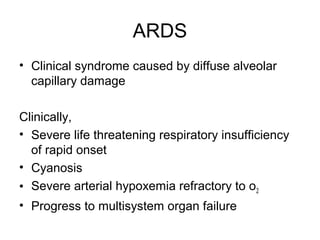
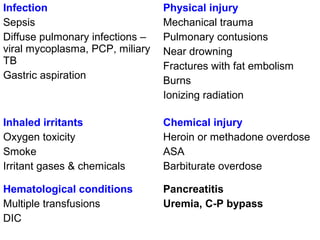
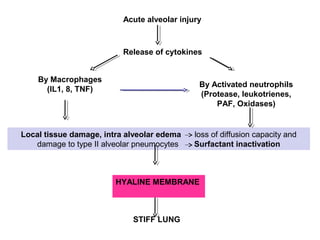
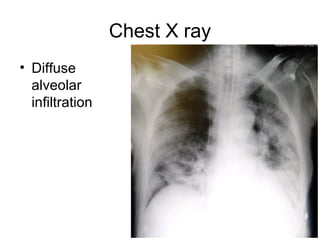
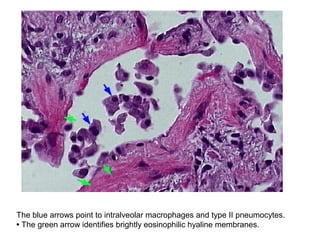
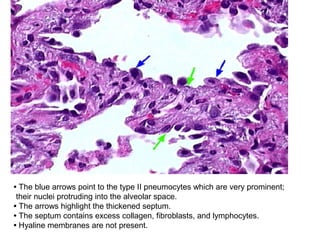
The document discusses various pulmonary diseases and abnormalities including atelectasis, acute respiratory distress syndrome (ARDS), and hyaline membrane disease. It describes the pathogenesis, clinical presentation, radiographic findings, and histopathology of these conditions. Regarding the case of the 7-year-old boy who inhaled a peanut, the document indicates that compression atelectasis is the most likely abnormality present, as a chest x-ray revealed mediastinal shift towards the side of the bronchial obstruction.