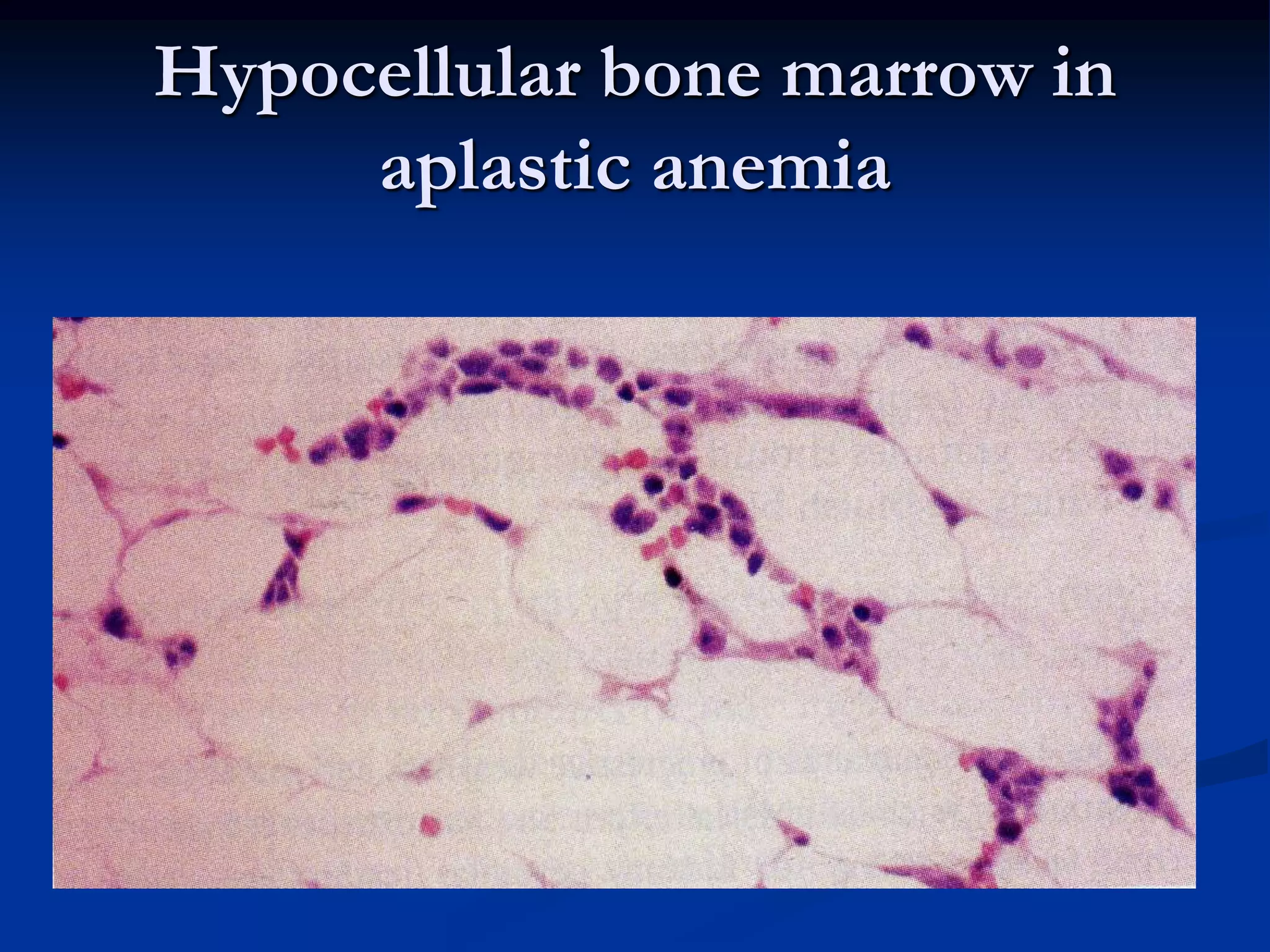
This document summarizes aplastic and hypoplastic anemias. Aplastic anemia is a life-threatening condition where the bone marrow fails to produce red blood cells, white blood cells, and platelets, leading to pancytopenia. It can be acquired through exposure to radiation, chemicals, infections or idiopathically. Congenital causes include Fanconi's anemia and familial aplastic anemia. Clinical manifestations include fatigue, pallor, infections, and bleeding. Treatment involves removing causative agents if known, blood transfusions, and bone marrow transplant. Related disorders with pancytopenia include myelodysplastic syndromes and pure red cell aplasia.