This document discusses the nature of disease and the human immune system. It covers several topics:
1) The various causes of disease including pathogens, genetic disorders, toxins, and physical damage. It also describes the mechanisms by which pathogens can cause disease.
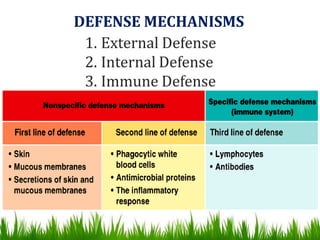
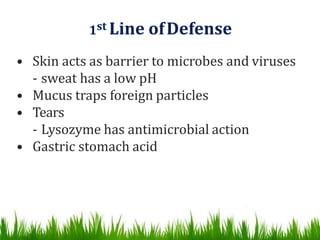
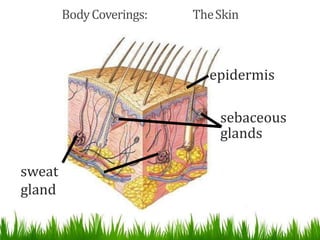
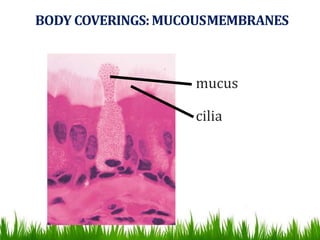
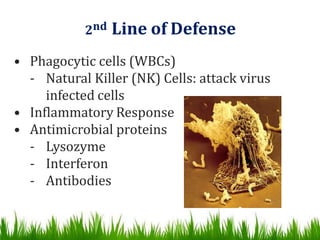
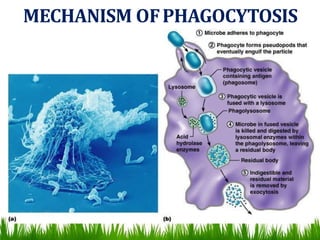
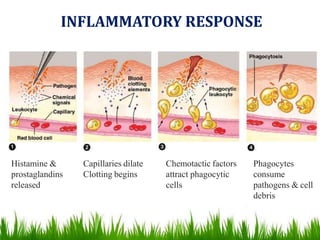
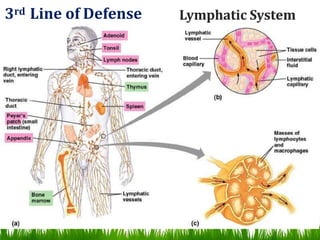
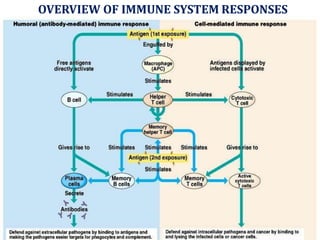
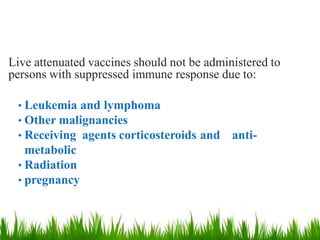
2) The immune system's three lines of defense - external barriers, internal inflammation and phagocytosis, and the adaptive immune system.
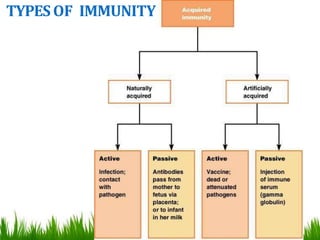
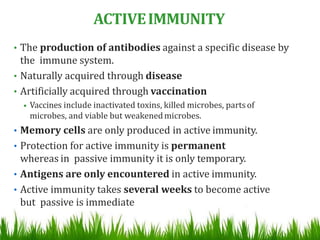
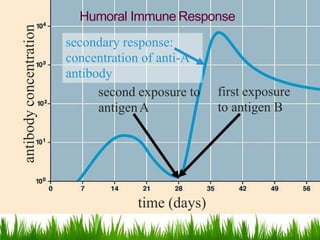
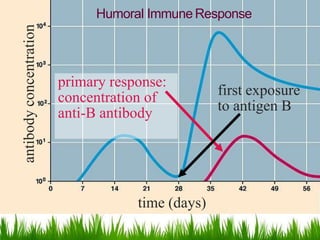
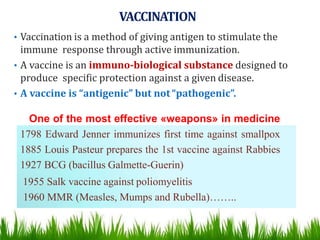
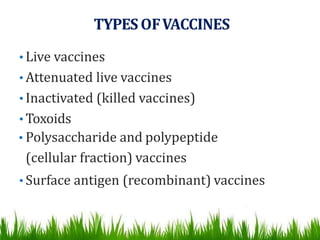
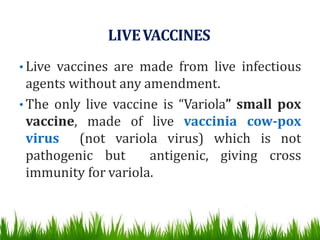
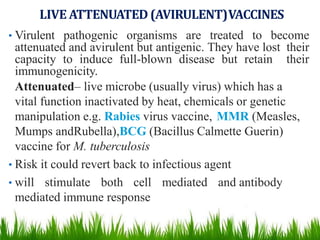
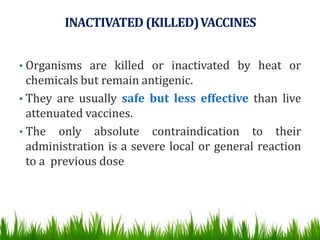
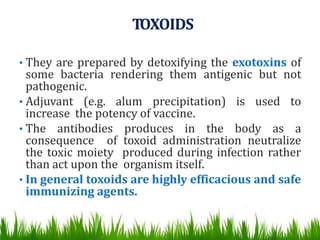
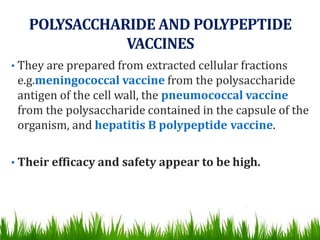
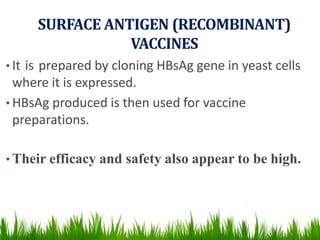
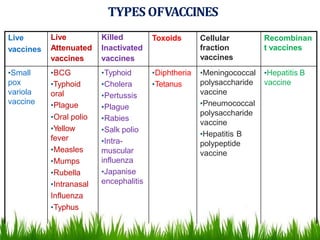
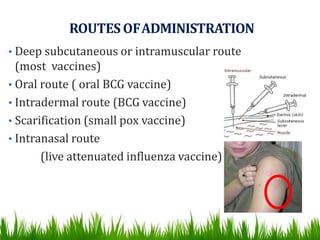
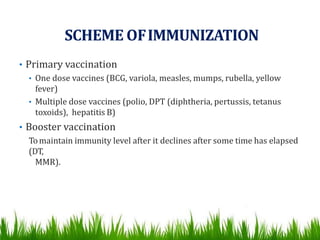
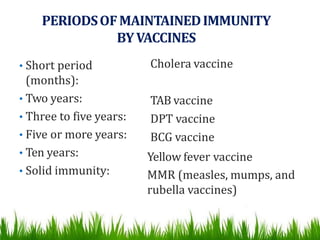
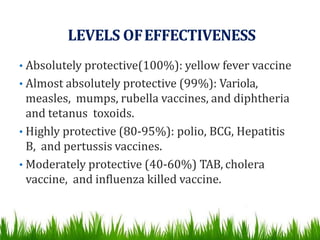
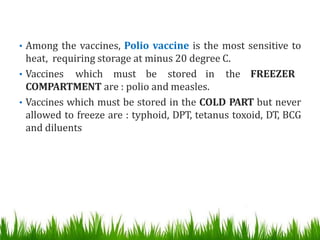
3) The different types of immunity, both natural and artificial, as well as active versus passive immunity. Vaccines are discussed as a way to artificially acquire active immunity.
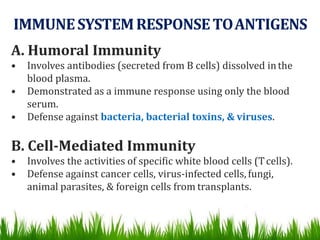
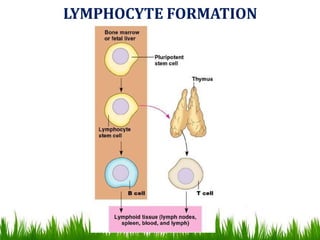
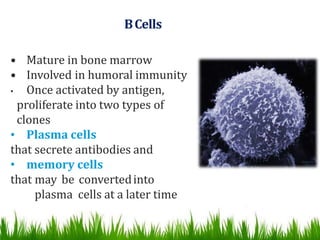
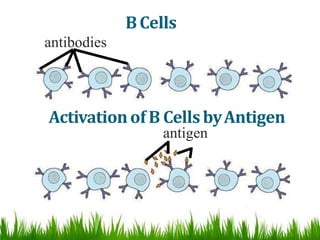
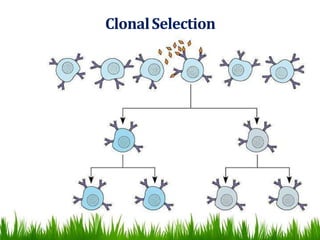
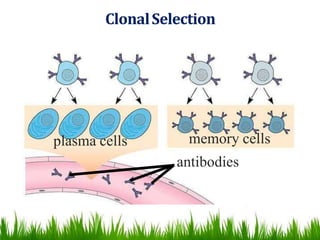
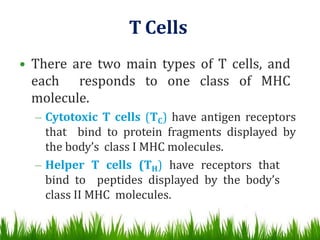
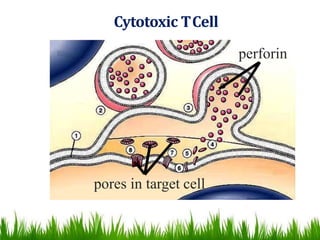
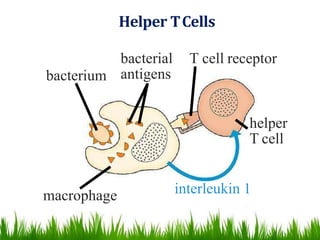
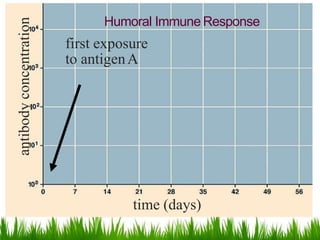
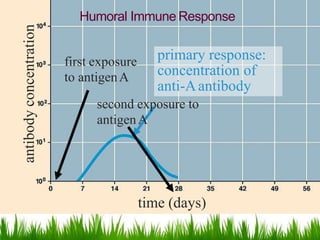
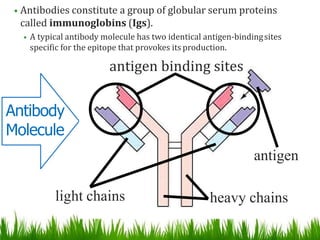
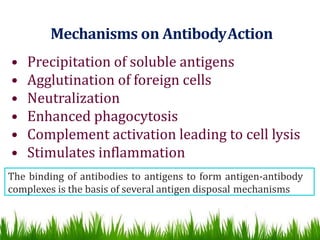
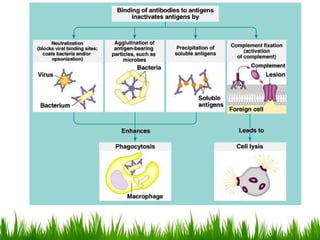
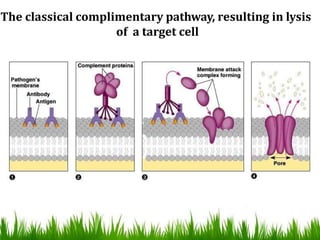
4) The key cells and responses of the immune system, including antibodies, B cells, T cells, and the differences between humoral