The document summarizes several common pediatric infections and exanthematous diseases:
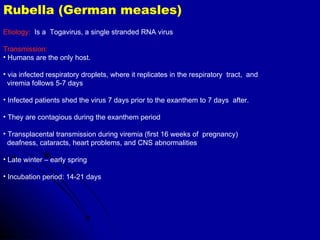
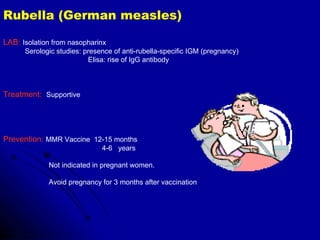
1) It discusses rubella (German measles), including its etiology, symptoms of a pink maculopapular rash and lymphadenopathy, and prevention through MMR vaccination.
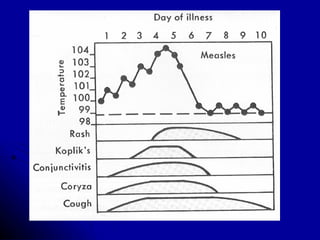
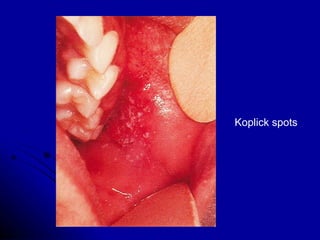
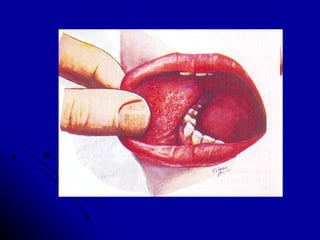
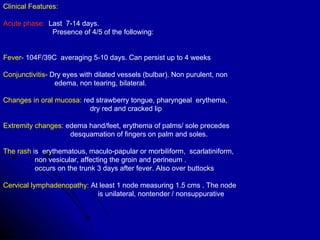
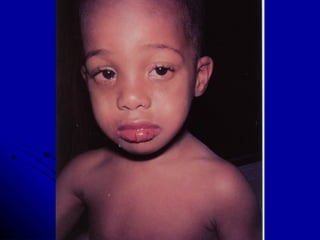
2) It describes rubeola (measles), caused by a paramyxovirus, with symptoms of a red maculopapular rash following a prodrome of fever and upper respiratory symptoms.
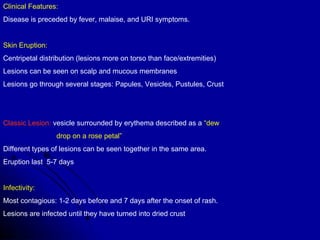
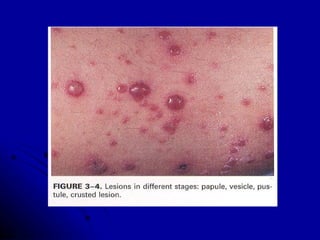
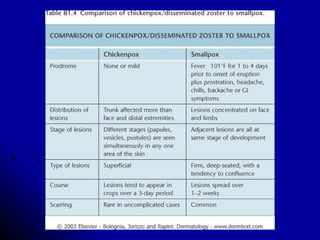
3) It briefly outlines varicella (chickenpox), caused by varicella-zoster virus, presenting with a centripetal vesicular rash that is highly contagious until lesions crust over.