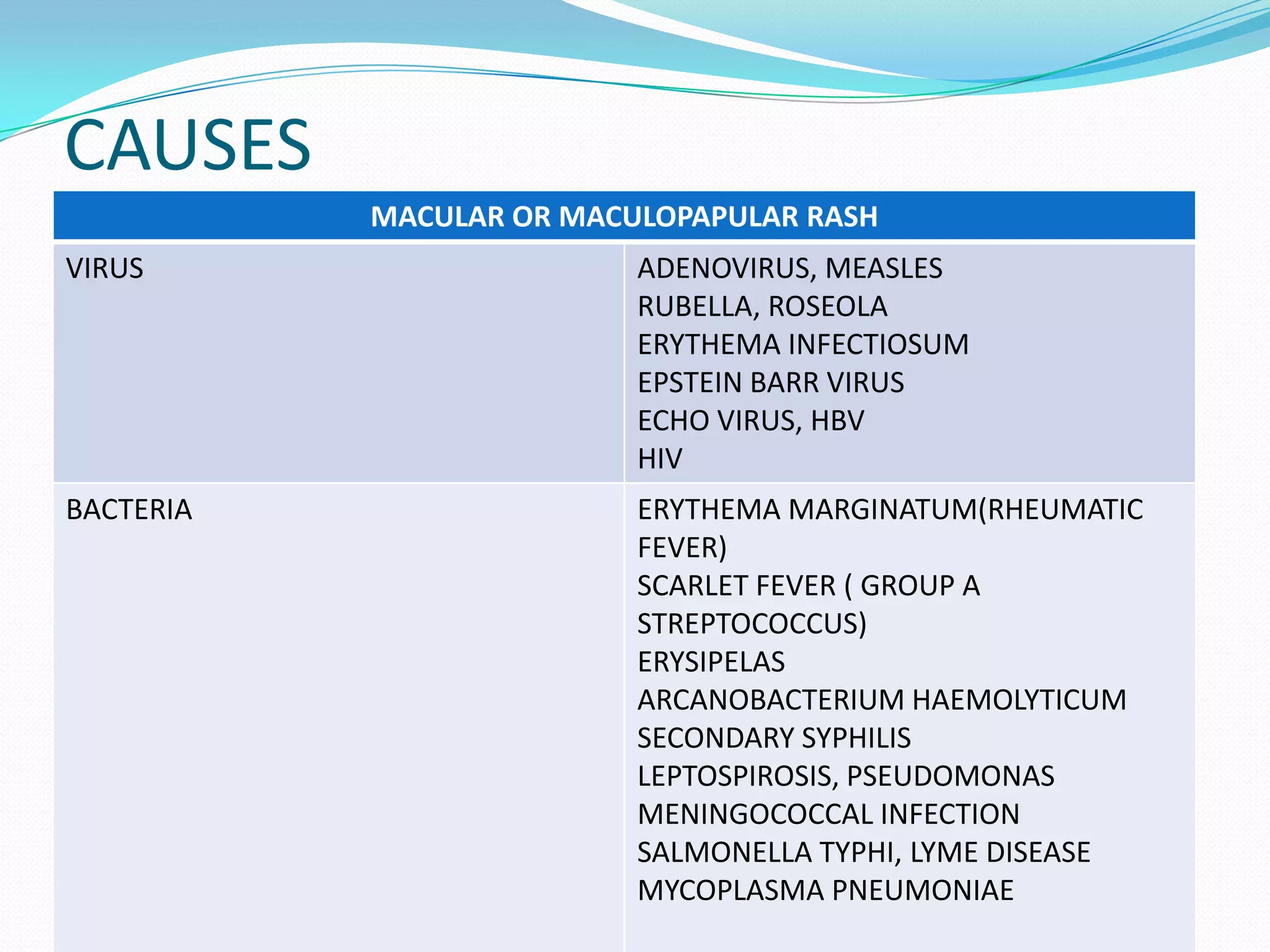
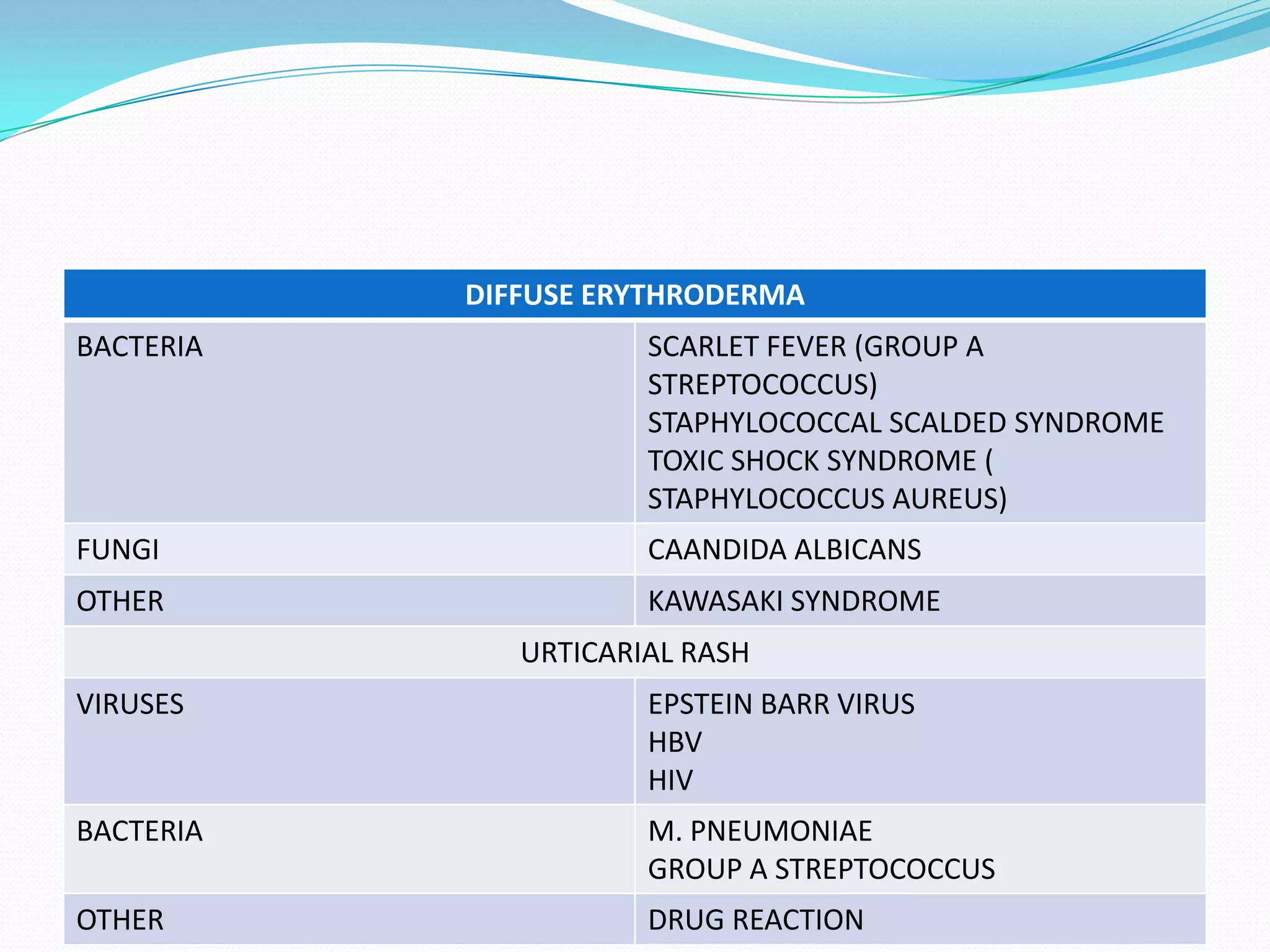
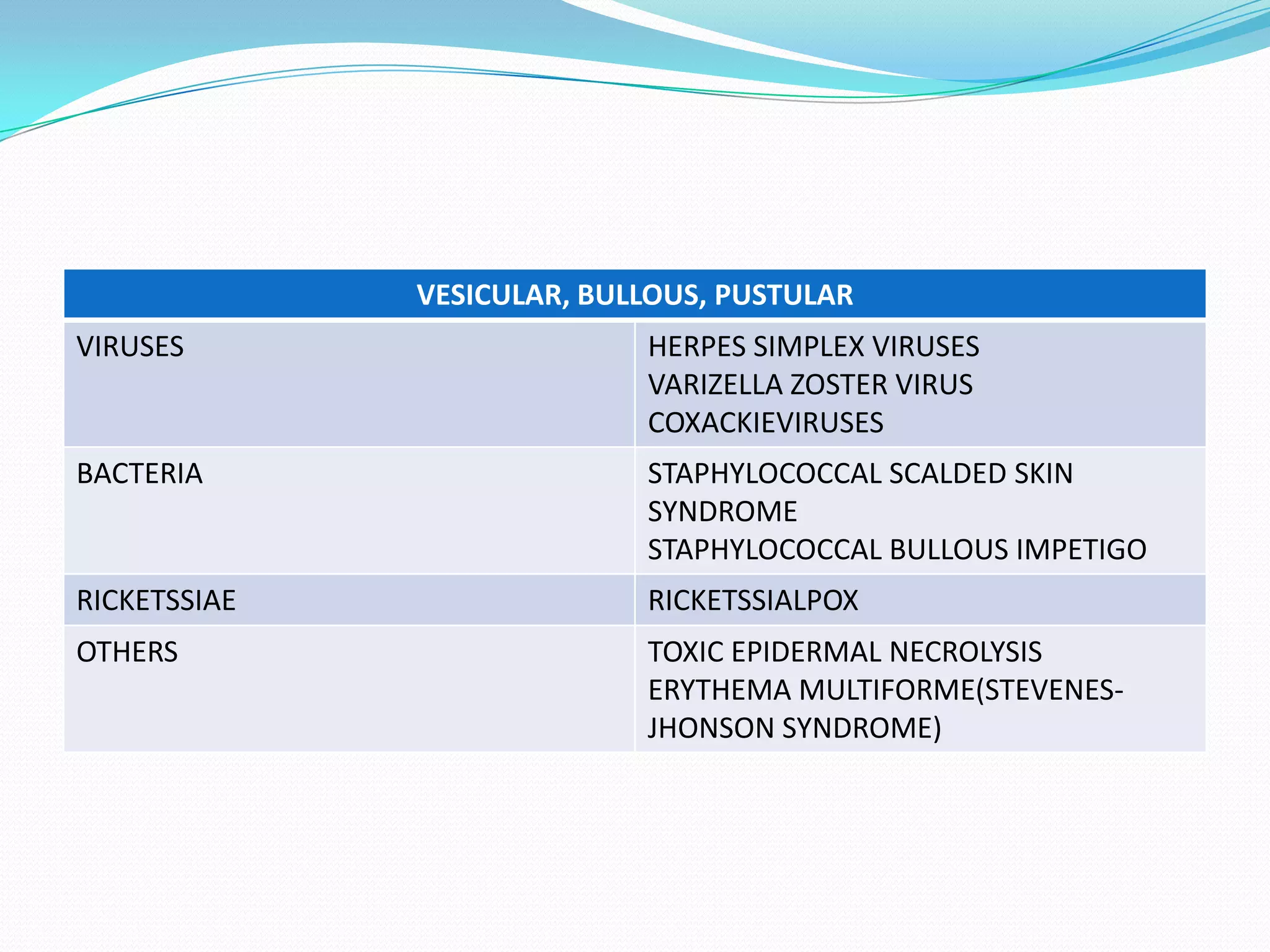
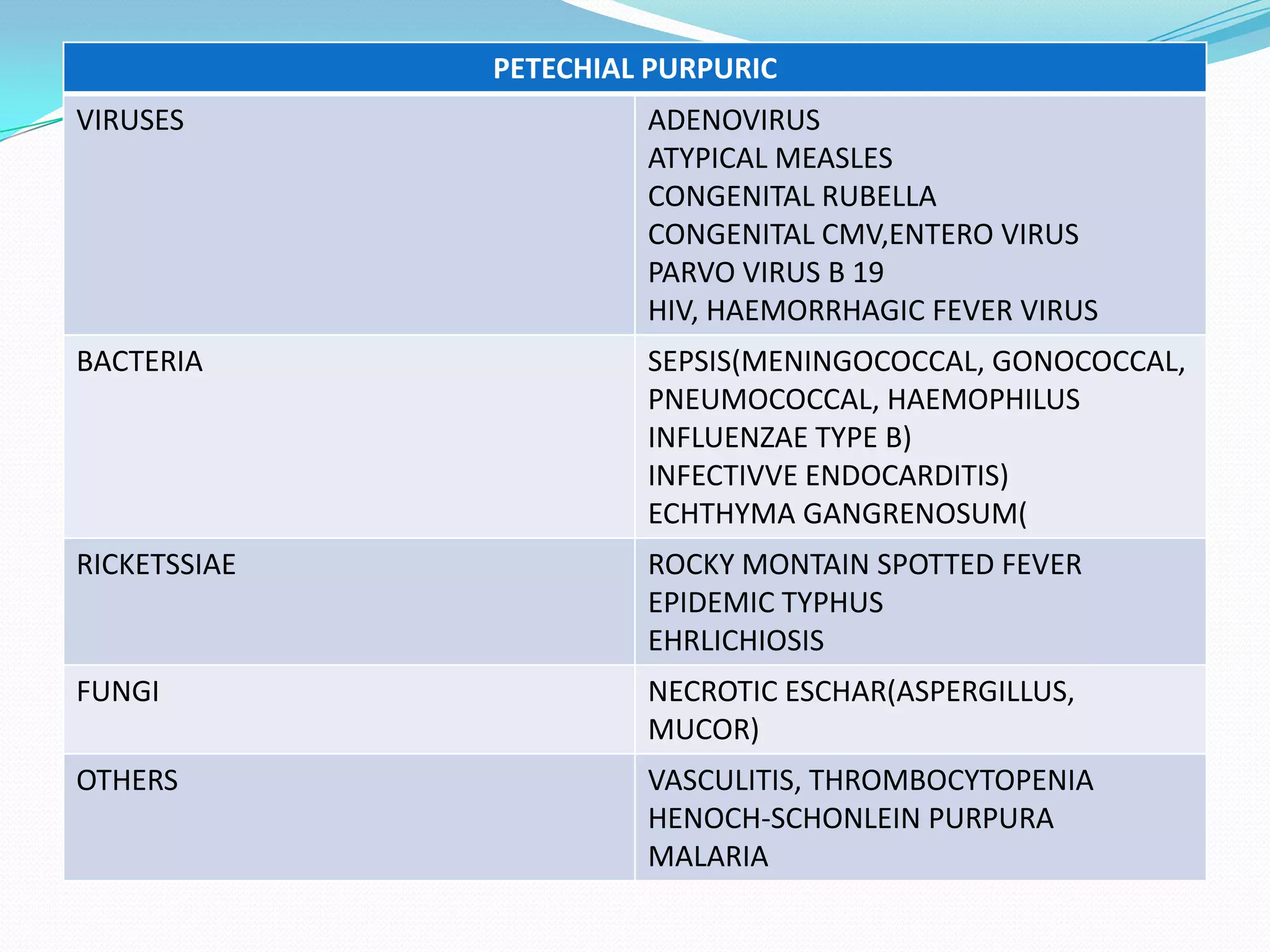
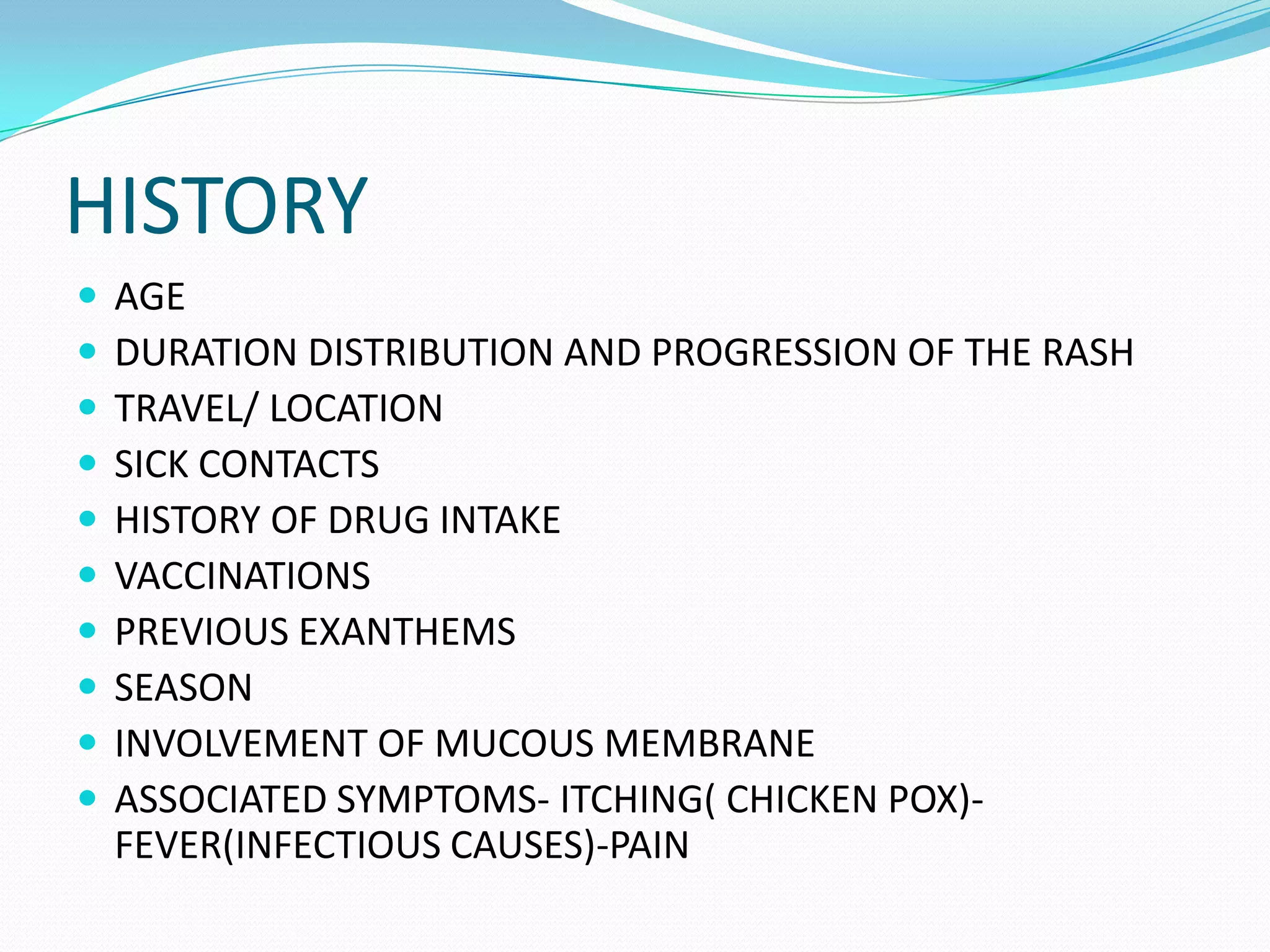
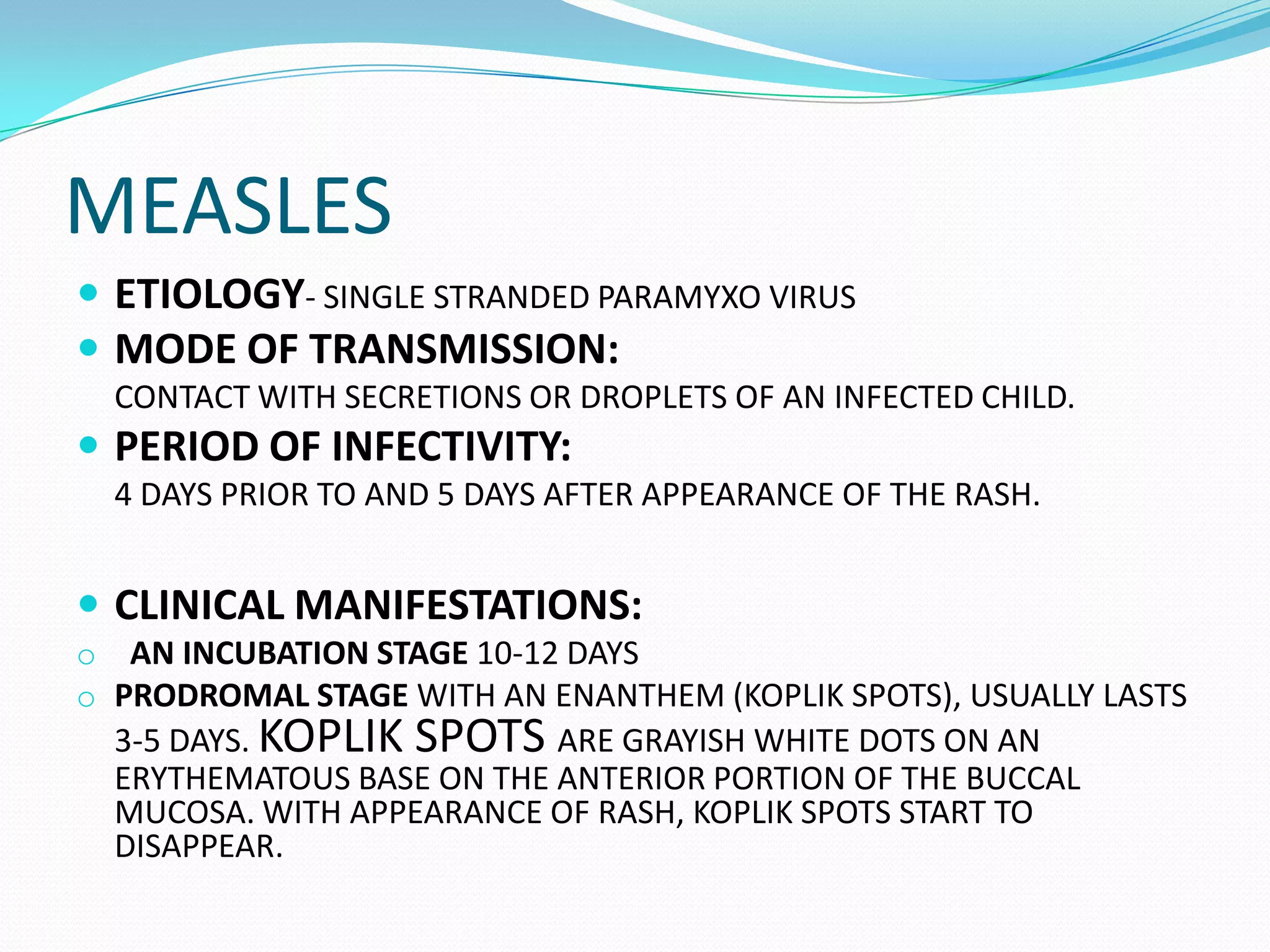
This document discusses several viral infections that can present with fever and rash, including measles, rubella, and chickenpox. It describes the causative agents, modes of transmission, incubation periods, clinical manifestations like rash appearance and progression, potential complications, treatments, and importance of vaccination.