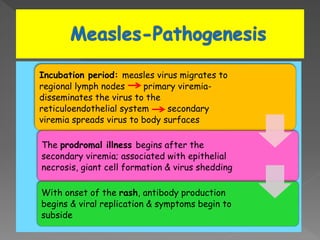
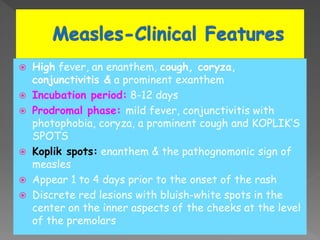
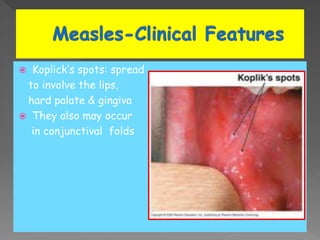
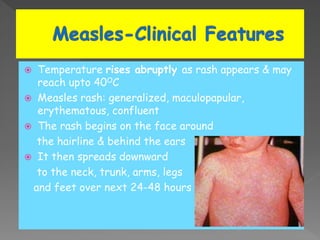
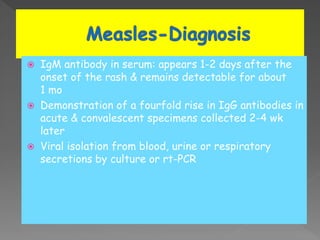
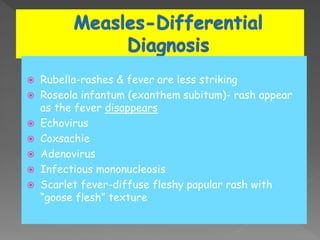
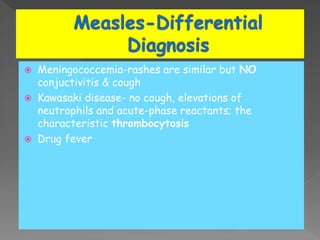
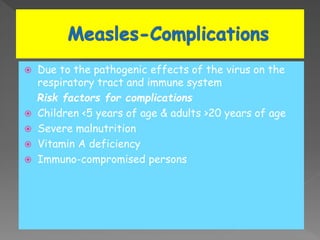
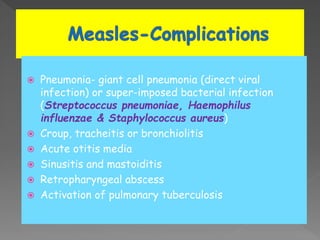
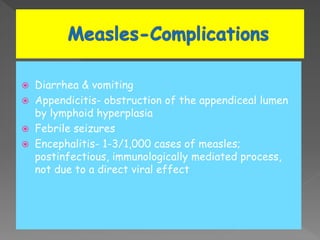
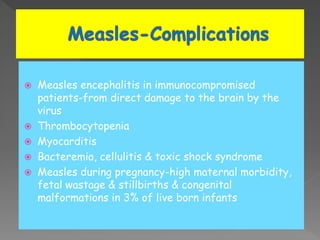
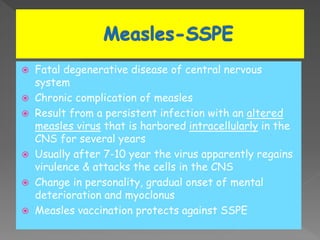
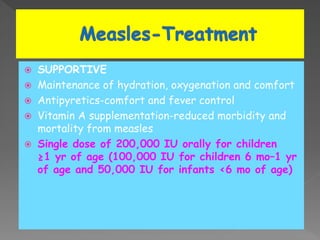
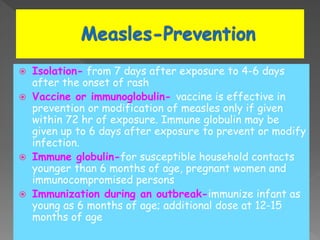
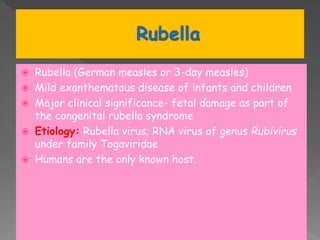
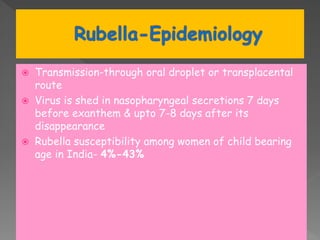
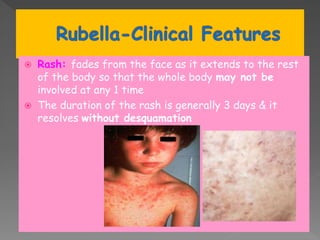
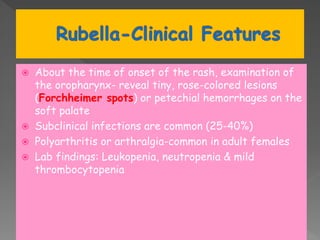
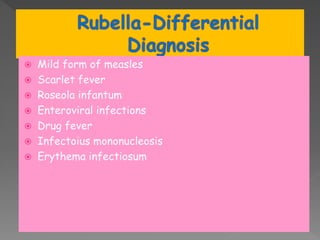
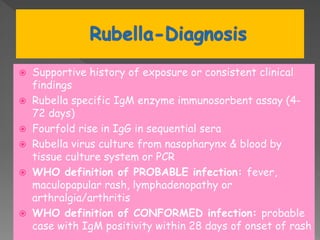
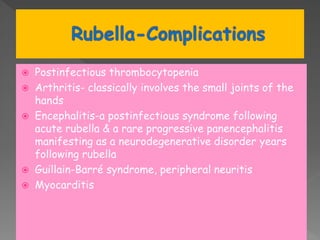
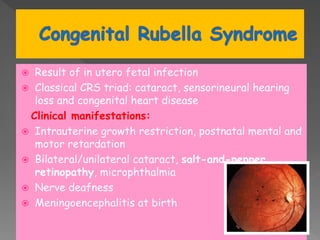
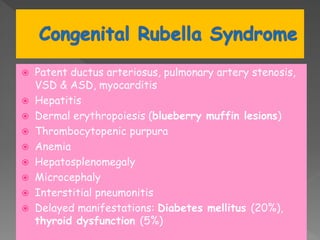
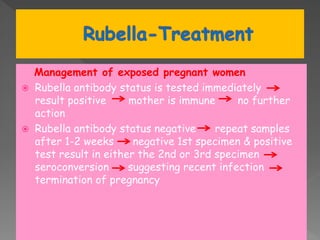
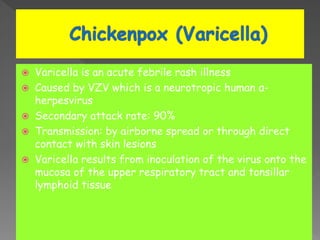
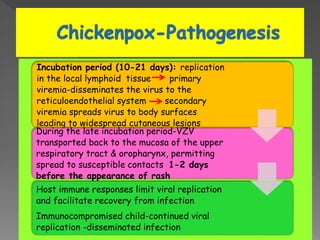
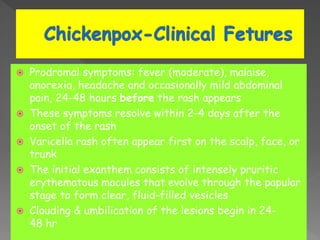
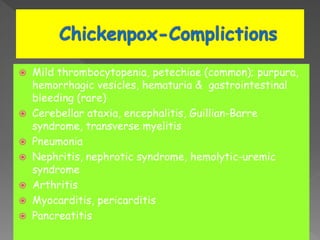
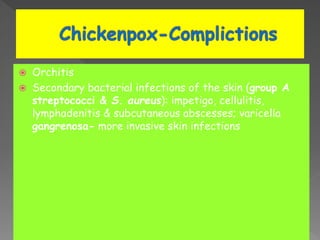
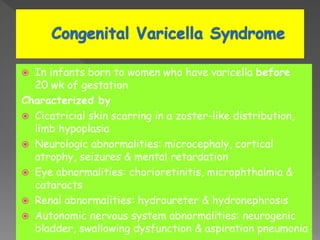
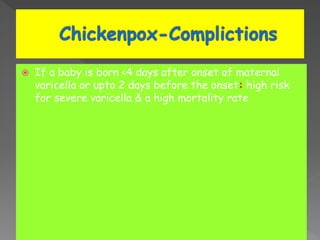
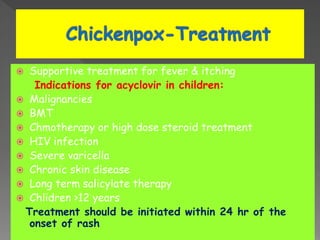
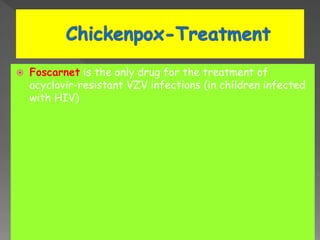
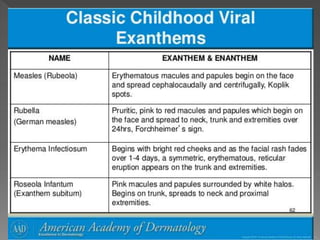
The document discusses the highly contagious viral diseases, measles and rubella, detailing their causative viruses, clinical presentations, and associated complications. It emphasizes the importance of vaccination to maintain high immunity levels and mitigate outbreaks, while describing the pathophysiology, symptoms like the characteristic rashes, and diagnostic criteria. Additionally, it addresses other conditions like varicella, including their transmission, treatment options, and the significance of supportive care for affected individuals.