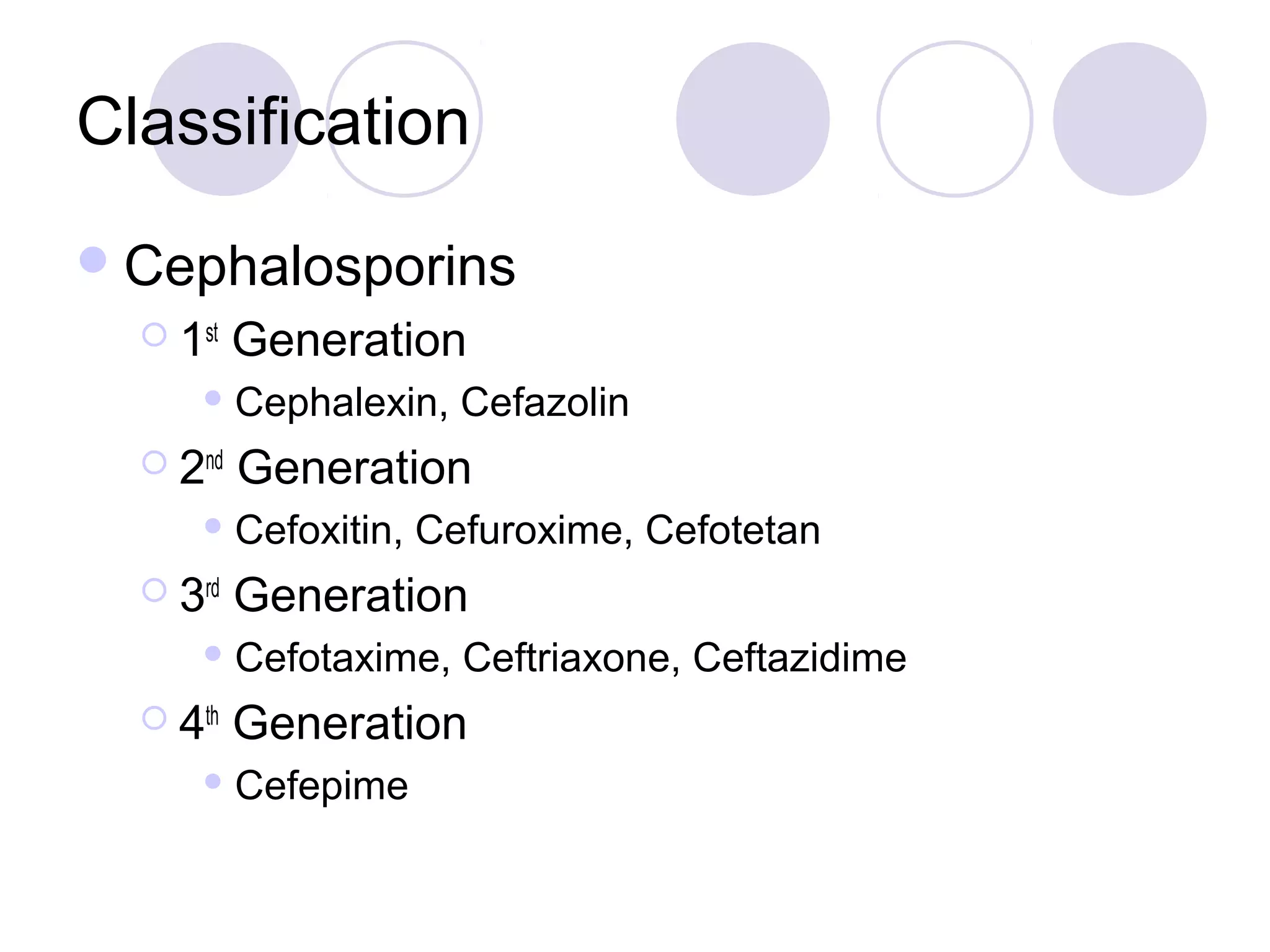
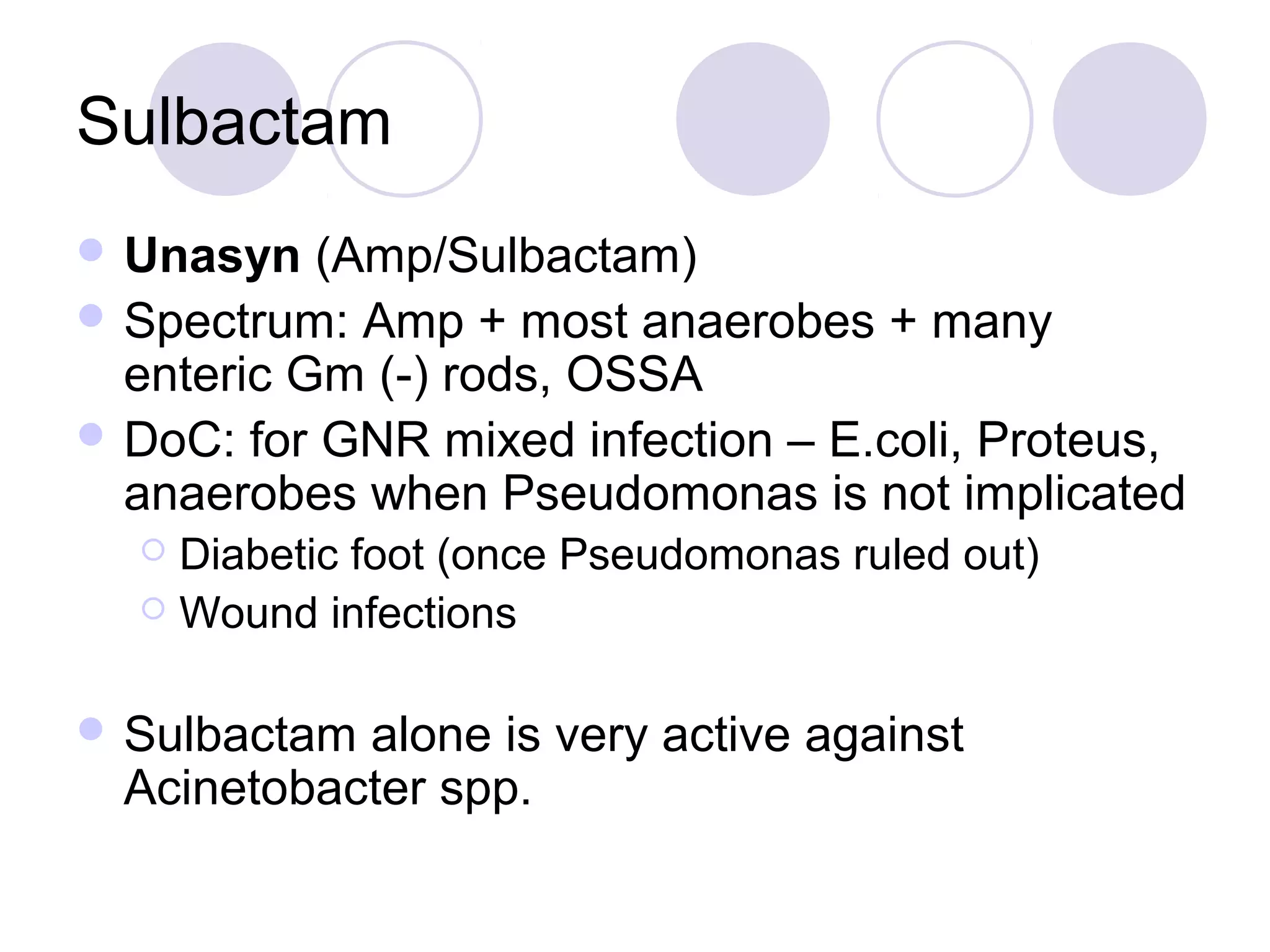
The document provides an overview of beta-lactam antibiotics, which are cell wall active agents that prevent bacterial cell wall synthesis and range from narrow to broad spectrum. It details their mechanisms of action, classifications (including penicillins and cephalosporins), and considerations for selection based on resistance and infection type. Adverse reactions, pharmacokinetics, and strategies for overcoming beta-lactamase resistance are also discussed.
![Classification
Penicillins
Natural penicillins
PenG, PenVK, Benzathine Pen, Procaine Pen
Aminopenicillins
Ampicillin, Amoxicillin
Anti-Staph penicillins
Oxacillin, Dicloxacillin
Anti-Pseudomonal
[Carboxy] Ticarcillin
[Ureido] Piperacillin](https://image.slidesharecdn.com/antibacterialssummary-121012065642-phpapp01/75/Antibacterials-summary-by-Laith-Yahya-9-2048.jpg)
![Penicillin G
AvailablePO, IM, IV (dosed in units)
Drug of Choice (DoC) [2-4 MU IV q4h]
T. pallidum, N. meningitidis, Group A Strep, and
Actinomycosis
Long-acting forms
Procaine PenG (12 hrs)
Benzathine Pen (5 days) [2.4 MU IM for syphilis]
Adverse Reactions – other than skin rash
Penicillin “serum sickness”/drug fever
Jarisch-Herxheimer reaction (1° and 2° syphilis)
Hemolytic anemia, pancytopenia, neutropenia](https://image.slidesharecdn.com/antibacterialssummary-121012065642-phpapp01/75/Antibacterials-summary-by-Laith-Yahya-11-2048.jpg)
![Ampicillin/Amoxicillin
Amp (IV, PO) Amox (PO)
Spectrum: PenG + H. flu and some E. coli
DoC: Listeria monocytogenes and
Enterococcus [Amp 2g IV q4h]
Dental Prophylaxis
Amox 1 gram PO x 1 prior to appt.
Integral in H. pylori regimens
ADRs
Non-allergic rashes (9%) – esp. when associated with a viral
illness (mononucleosis - EBV)
Amox better tolerated PO and better absorbed (Amp must be
taken on empty stomach)](https://image.slidesharecdn.com/antibacterialssummary-121012065642-phpapp01/75/Antibacterials-summary-by-Laith-Yahya-12-2048.jpg)
![Oxacillin
IV
DoC – MSSA, MSSE [2g IV q4h]
Actually less active against Pen susceptible isolates
than Pen
More active than Vanc vs. MSSA
Significant hepatic metabolism
No need to dose adjust for renal impairment
ADRs
Hepatotoxicity (cholestatic hepatitis)
Neutropenia
Kernicterus in neonates](https://image.slidesharecdn.com/antibacterialssummary-121012065642-phpapp01/75/Antibacterials-summary-by-Laith-Yahya-13-2048.jpg)
![Cephalexin/Cefazolin
PO/IV
Stablevs Staph penicillinase
Spectrum: MSSA, PSSP, most E. coli, and some
Klebs
Can be dose thrice weekly in HD pts
[1.5 grams IV TIW]
DoC:surgical prophylaxis, bacterial peritonitis in
CAPD pts [1 gm in the dwell bag]
ADRs
Positive Coombs’ test (though, hemolytic anemia is
rare)](https://image.slidesharecdn.com/antibacterialssummary-121012065642-phpapp01/75/Antibacterials-summary-by-Laith-Yahya-21-2048.jpg)