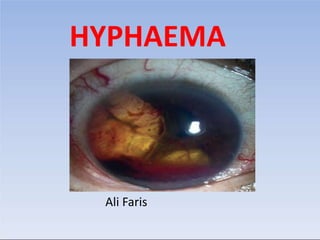
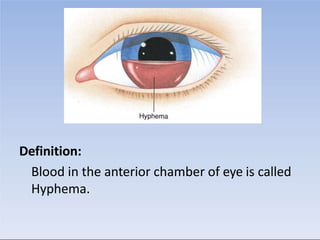
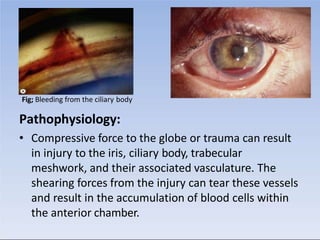
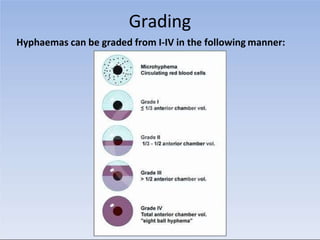
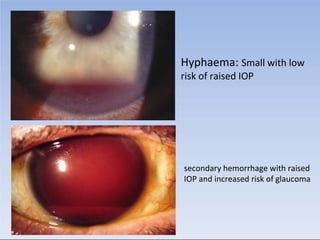
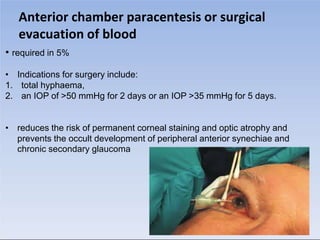
This document defines hyphaema as blood in the anterior chamber of the eye. It can result from compressive trauma that injures blood vessels in the iris, ciliary body, or trabecular meshwork. Hyphaema is classified based on etiology (traumatic, medical conditions, etc.) and severity (mild, moderate, severe). Presentation includes blurry vision, pain, and blood visible in the anterior chamber. Examination involves assessing injury, vision, pressure, and ruling out other issues. Treatment focuses on preventing increased pressure through medications, limiting activity, and sometimes surgery to remove blood if pressure remains high.