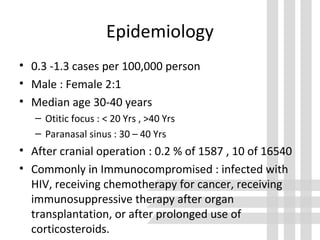
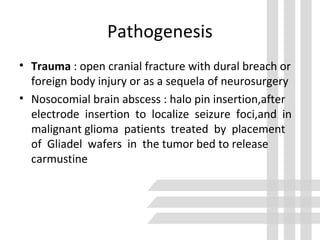
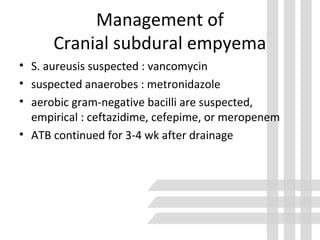
This document discusses brain abscess, cranial subdural empyema, and epidural abscess. It covers the epidemiology, etiology, pathogenesis, clinical findings, diagnosis, and management of these conditions. Brain abscesses are typically caused by bacteria spreading from contiguous sites of infection or through the bloodstream. Clinical findings depend on the location and size of the abscess. Diagnosis involves neuroimaging and culture of aspirated contents. Treatment involves antibiotics and sometimes surgery. Outcomes depend on early diagnosis and treatment.