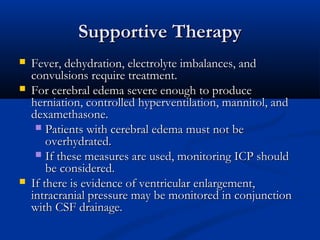
Brain abscess is a focal infection within the brain parenchyma, typically surrounded by a capsule. It has an incidence of 0.3-1.3 per 100,000 people per year. Common causes include direct spread from a contiguous infection like sinusitis, hematogenous spread from infections elsewhere in the body, and head trauma. Clinical presentation is usually gradual onset of nonspecific symptoms like headache, fever, and focal neurological deficits. Diagnosis involves neuroimaging like MRI or CT scan showing a brain lesion, and microbiological evaluation of aspirated pus. Treatment consists of high dose intravenous antibiotics plus surgical drainage of the abscess. Prognosis depends on causative organism and ability to control infection, with a mortality rate of