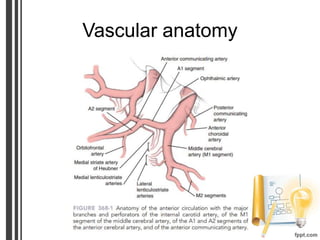
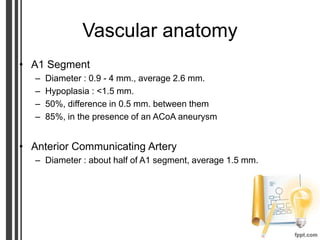
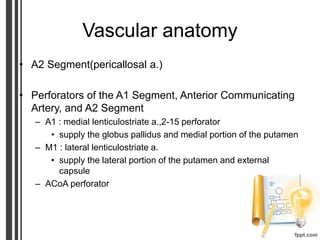
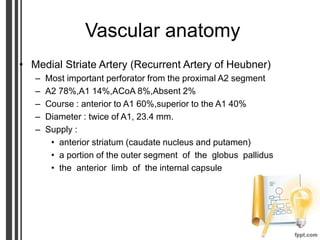
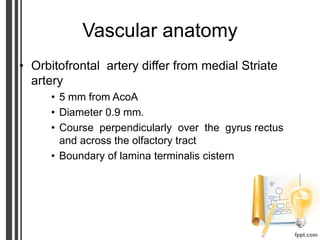
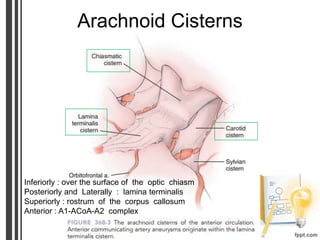
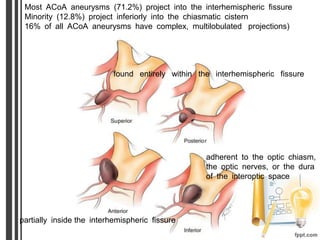
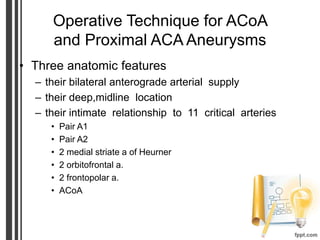
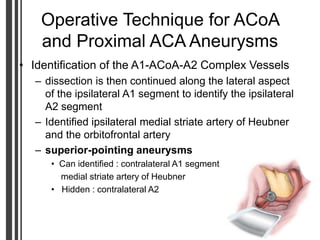
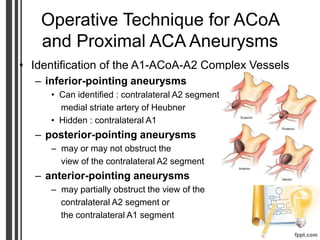
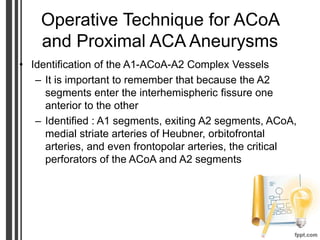
1) Anterior communicating artery aneurysms are located at the junction between the paired anterior cerebral arteries. They have complex anatomy and relationships with nearby vessels.
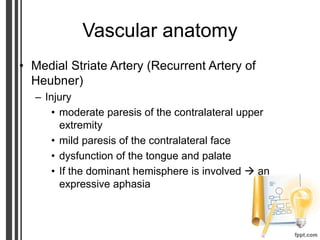
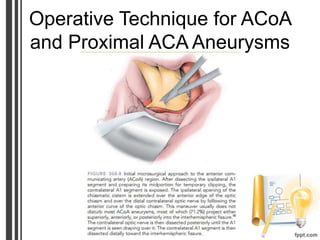
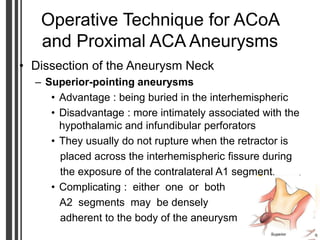
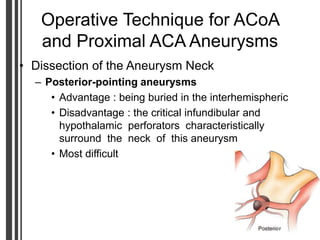
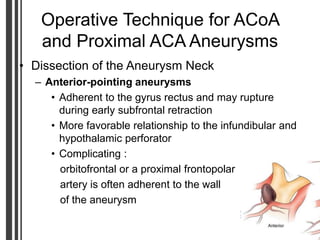
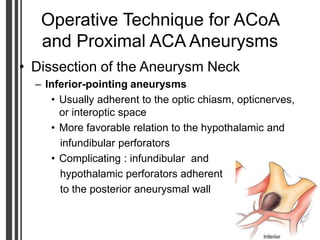
2) Surgical clipping requires meticulous dissection to safely access and clip the aneurysm neck while preserving critical perforating arteries.
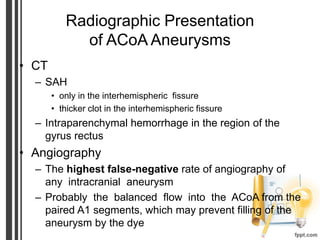
3) Both microsurgery and endovascular coiling are treatment options, with endovascular being relatively contraindicated for aneurysms with an absent A1 segment or complex dome/neck anatomy. Small, anteriorly-projecting aneurysms have higher coiling success rates.