This document provides information on brain abscesses, including their history, epidemiology, pathogenesis, clinical presentation, investigations, management, and surgical treatment. Some key points:
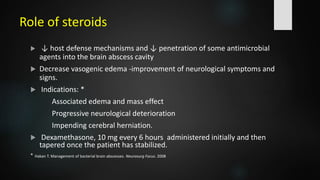
- Brain abscesses are focal intracranial infections that start as cerebritis and evolve into a collection of pus surrounded by a capsule. The most common causes are spread from a contiguous infection or hematogenous dissemination.
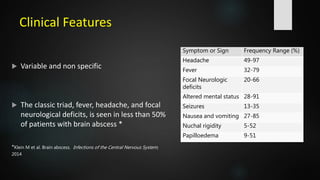
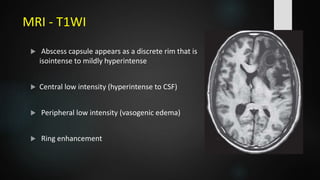
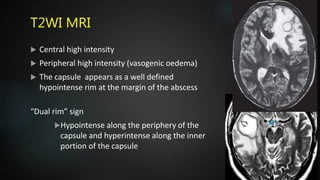
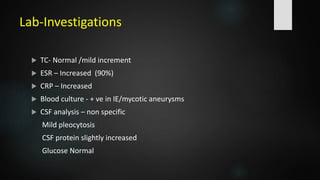
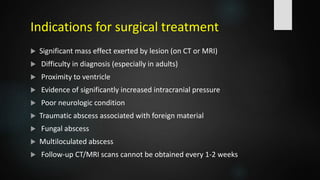
- Clinical features are often non-specific but may include headache, fever, focal neurological deficits, and altered mental status. Investigations like CT and MRI are used to identify location, size, and stage of the abscess.
- Treatment involves antibiotics along with surgical evacuation for abscesses over 2.5cm