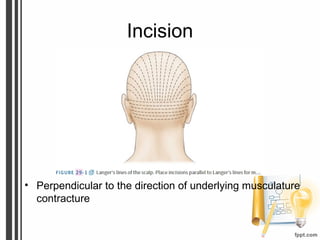
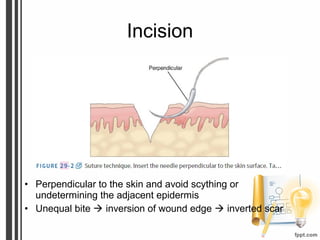
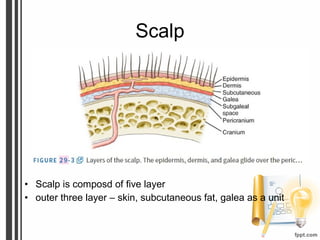
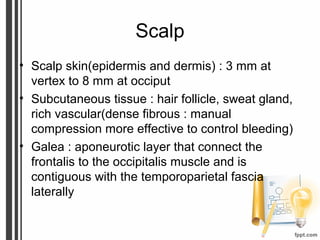
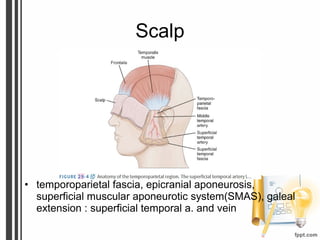
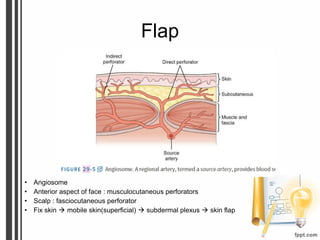
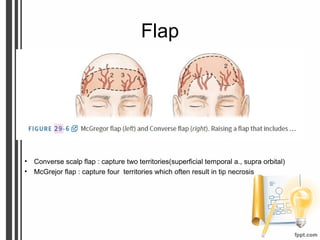
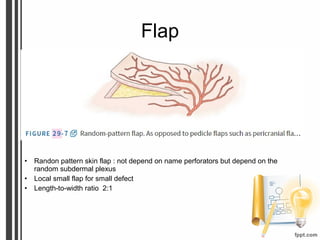
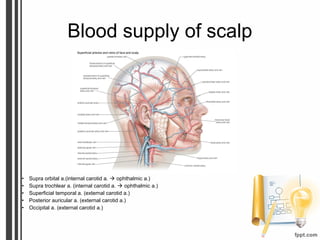
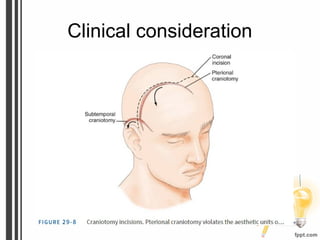
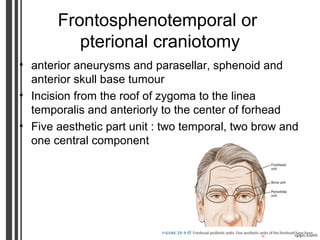
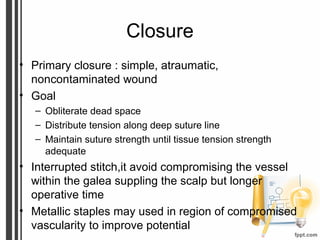
This document discusses incision and closure techniques for surgery involving the scalp. It covers wound healing phases, antibiotic indications, scalp anatomy including blood vessels, and closure considerations. The scalp has 5 layers (skin, fat, galea, fascia, muscle) supplied by temporal, occipital and frontal arteries. Common craniotomies like frontotemporal involve coronal incisions along aesthetic units. Subtemporal and suboccipital approaches also discussed. Primary closure aims to eliminate dead space and distribute tension until tissue strength recovered.