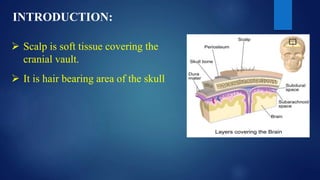
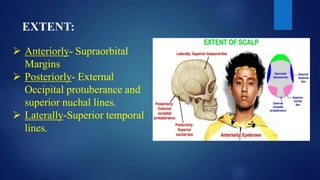
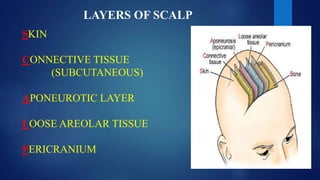
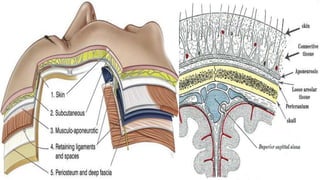
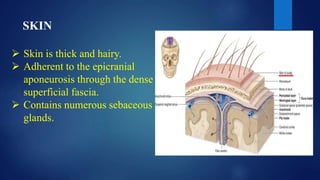
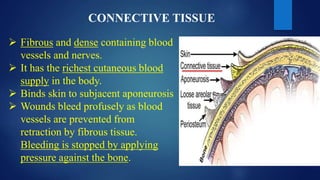
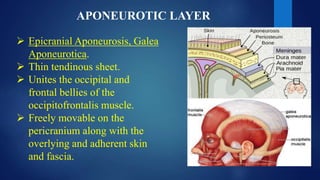
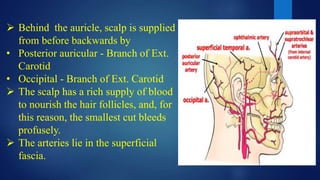
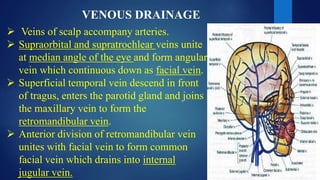
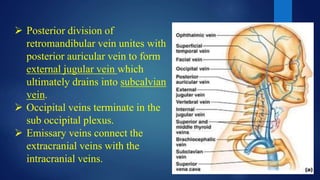
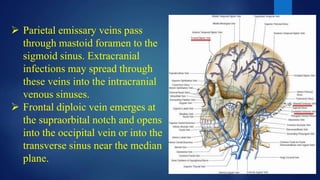
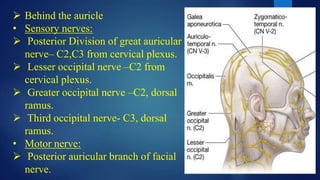
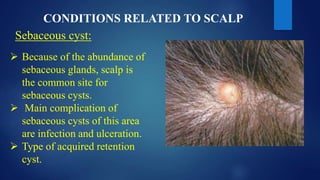
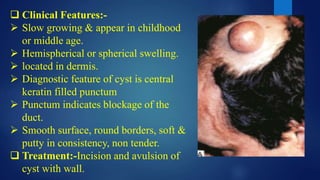
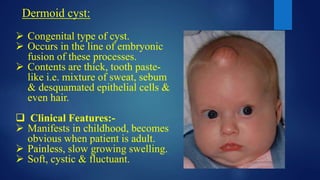
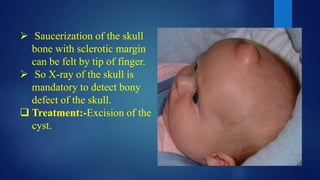
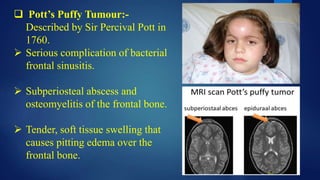
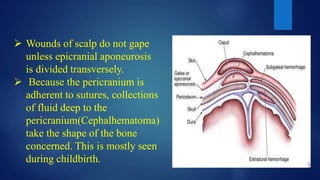
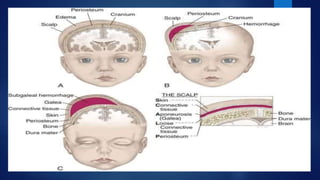
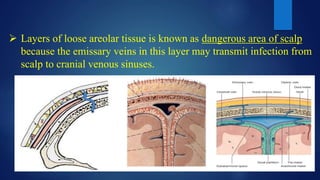
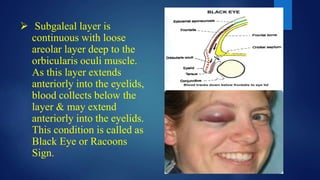
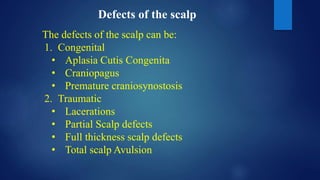
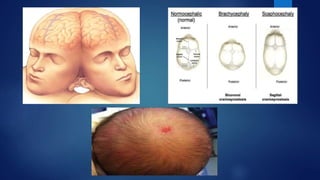
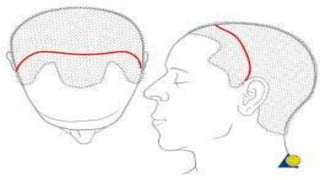
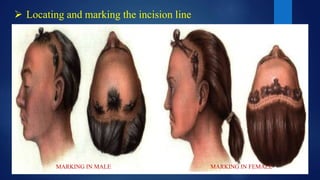
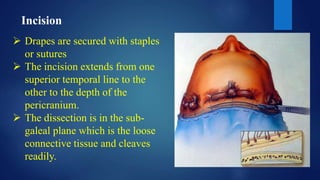
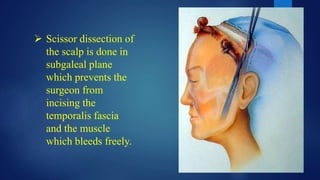
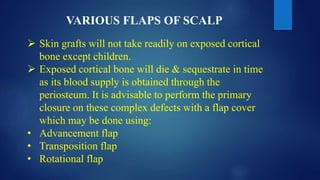
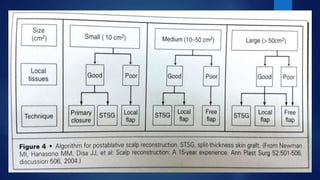
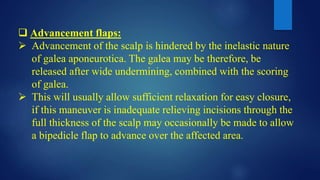
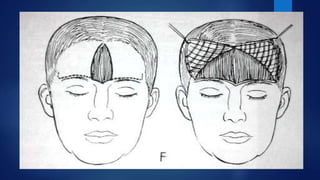
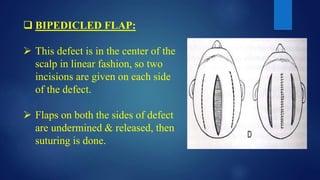
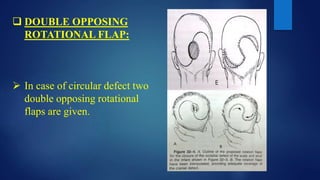
The document provides information on the anatomy of the scalp, including its layers, blood supply, drainage and innervation. It discusses several clinical conditions that can affect the scalp, such as sebaceous cysts and Pott's puffy tumor. It also describes treatments for scalp wounds and defects, including various local flaps and free tissue transfers. Coronal and hemi-coronal incisions are presented as approaches commonly used for scalp surgery.