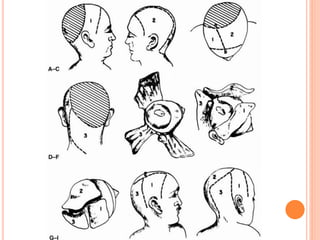
The document presents a comprehensive overview of scalp defects, detailing the anatomy of the scalp and the various layers involved, including the galea aponeurotica and pericranium. It discusses causes of scalp defects, treatment options such as skin grafting and local flaps, and techniques for proper management, including tissue expansion and flap surgery. Additionally, it outlines considerations for successful reconstruction and potential complications associated with different surgical methods.



























![GALEAL FLAP
Based on STA
galeal flap is commonly based on a named scalp vessel or combination of
vessels.
Flap length can often cross the midline
Can be elevated with frontalis muscle of the forehead to reconstruct the
anterior cranial base.
Can be taken with bone [vascularized cranial bone for reconstruction about
the orbit and facial skeleton ]
Subgaleal areolar tissue can be raised with the underlying periosteum as a
turnover flap to provide vascularized coverage for denuded calvaria](https://image.slidesharecdn.com/scalpdefects-210623023002/85/Scalp-defects-36-320.jpg)




![REGIONAL FLAP
Trapezius flap : type 2
For occipital defects
blood supply :- transverse cervical
dorsal scapular
occipital arteries
Pattern :
Transverse flap : upper fibres [A/w shoulder drop]
Vertical flap : middle and lower fibres
8-10 cm donor defect can be closed primarily](https://image.slidesharecdn.com/scalpdefects-210623023002/85/Scalp-defects-41-320.jpg)



![LD FLAP [PEDICLED /FREE]
By passage of the muscle through the axilla,
defects in the orbit and temporal bone can be
repaired.](https://image.slidesharecdn.com/scalpdefects-210623023002/85/Scalp-defects-45-320.jpg)

![FREE TISSUE TRANSFER
LD [Flap of choice for large defects]
RFF
ALT
Omental Flap with STSG
Free temporo-occipital scalp flap for free hair
baring tissue transfer](https://image.slidesharecdn.com/scalpdefects-210623023002/85/Scalp-defects-47-320.jpg)
![CHECKLIST
I. Named vessel included?
II. Native hairline preserved ?
III. Mode of injury?
IV. Inherent inelasticity of galea and mobile parietal and
occipital region [neck]
V. Donor site : less sensitive cosmetically?](https://image.slidesharecdn.com/scalpdefects-210623023002/85/Scalp-defects-48-320.jpg)