This document discusses the principles of craniotomy, including:
1. A brief history of craniotomy from ancient times to modern techniques.
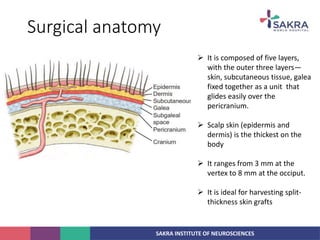
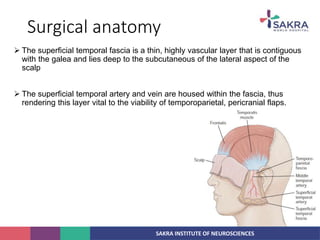
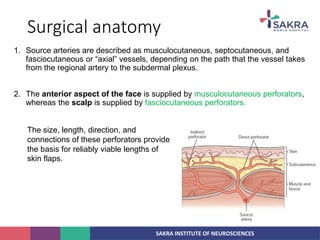
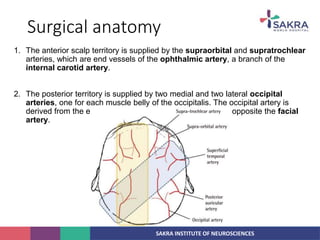
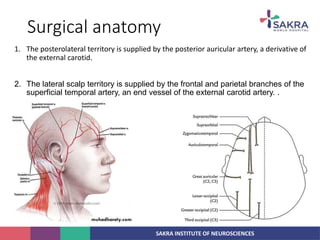
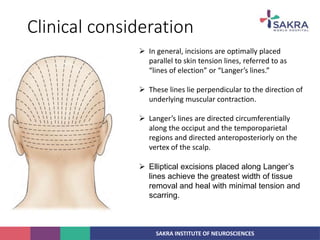
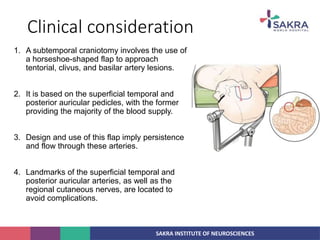
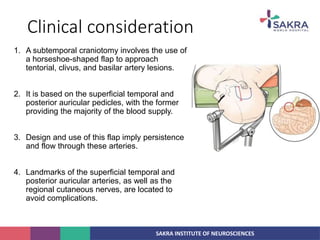
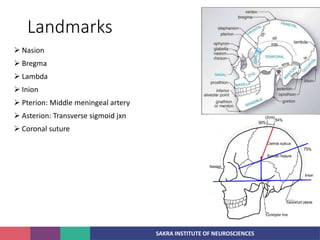
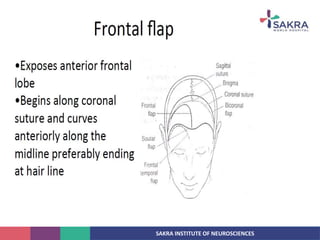
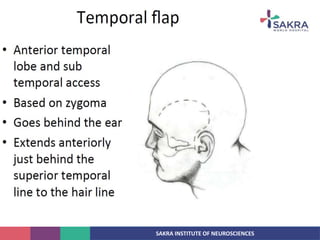
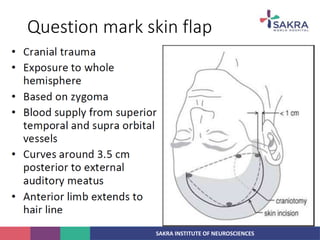
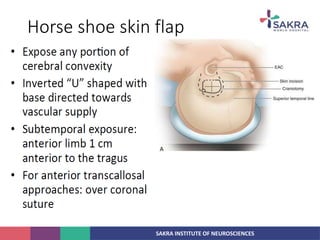
2. The anatomy of the scalp and neurovascular structures important for craniotomy.
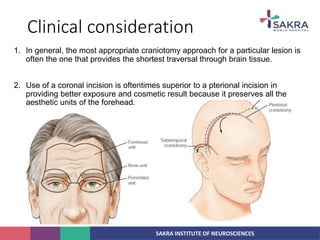
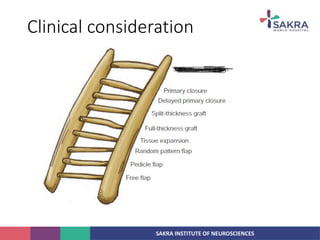
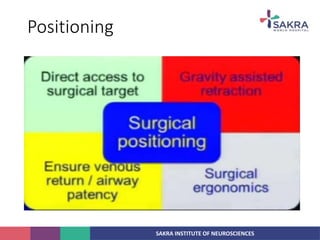
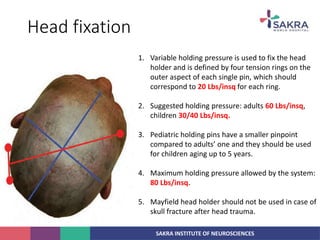
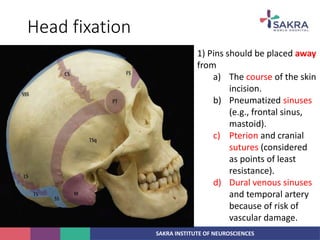
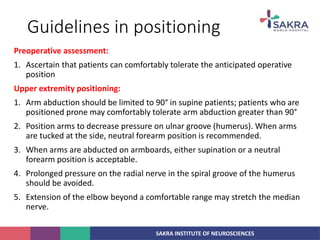
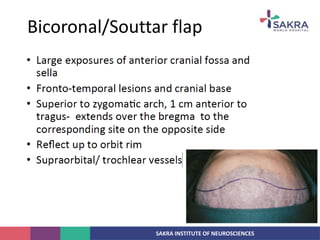
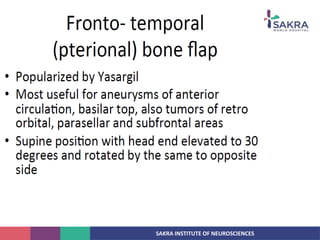
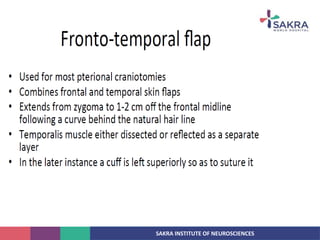
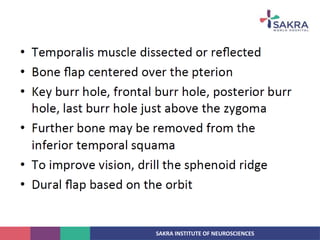
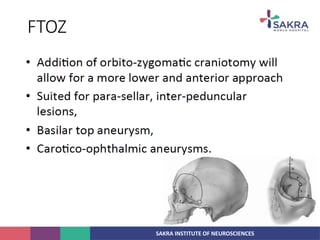
3. Key considerations for patient positioning, head fixation, incision planning, and wound closure to optimize exposure and outcomes.
4. General principles for craniotomy including adequate exposure, minimizing brain retraction and damage to surrounding structures, and preserving scalp flap vascularity.