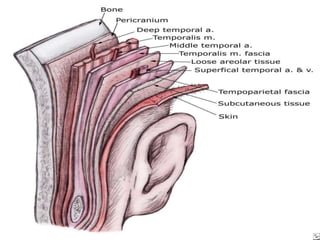
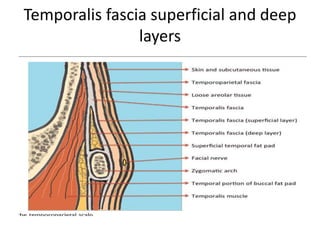
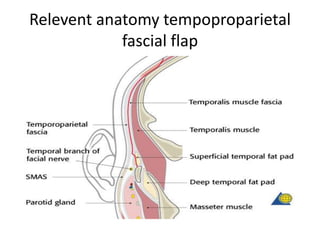
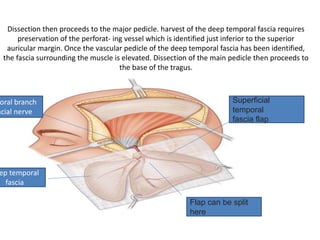
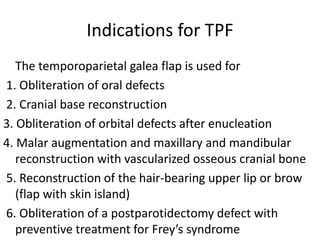
The temporoparietal fascial flap (TPF) uses fascia from the scalp which is supplied by the superficial temporal artery. It can be used as a pedicled or free flap for reconstruction of facial, orbital, and skull defects. The relevant anatomy is described including landmarks for incision and dissection. Indications include reconstruction of oral, orbital, and cranial defects. Advantages are an easy harvest with a reliable vascular pedicle and low donor site morbidity. Disadvantages include a short pedicle length and potential scarring or alopecia at the donor site.