This document discusses the anatomy, pathology, imaging characteristics, differential diagnosis, and surgical approaches related to the cerebellopontine angle. Key points include:
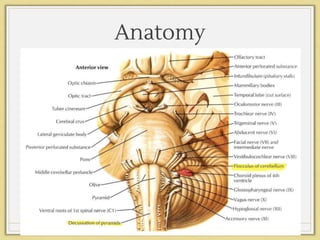
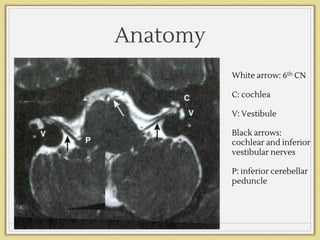
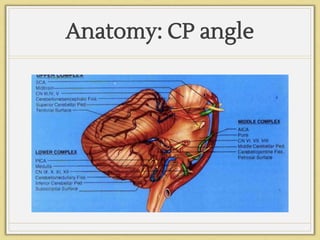
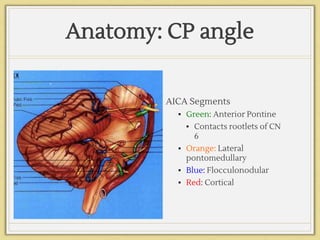
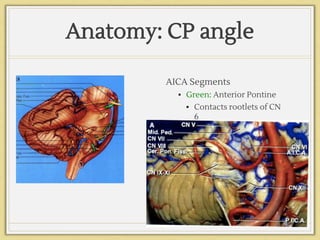
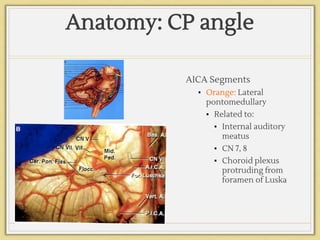
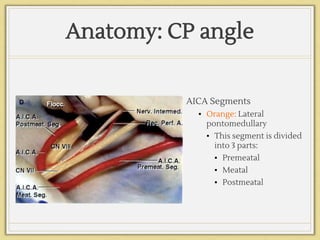
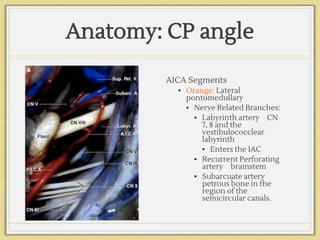
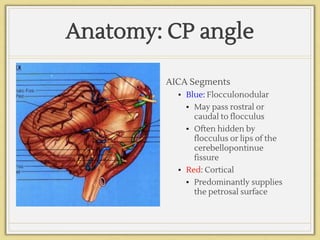
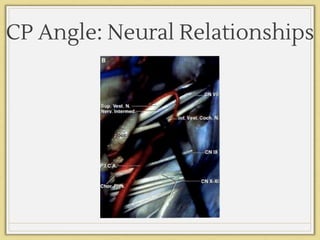
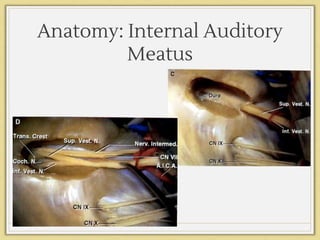
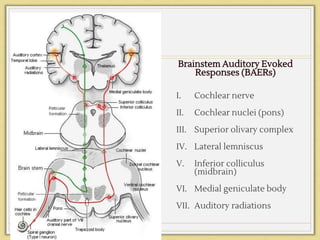
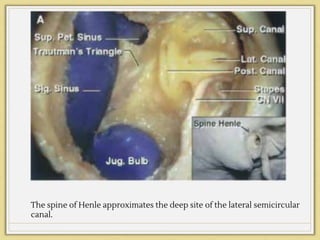
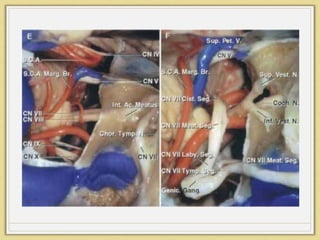
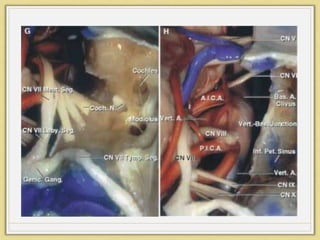
- The cerebellopontine angle contains 3 neurovascular complexes supplied by the superior, anterior inferior, and posterior inferior cerebellar arteries.
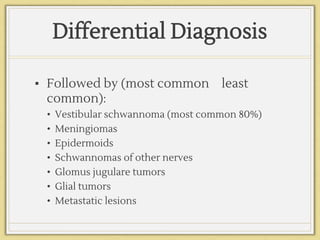
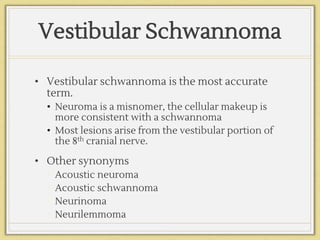
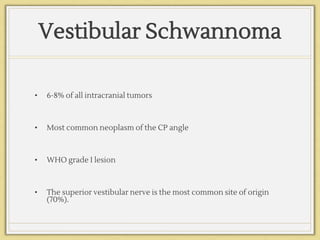
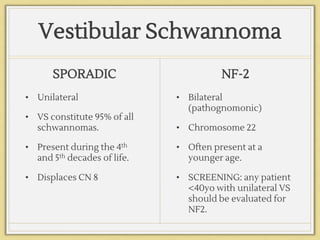
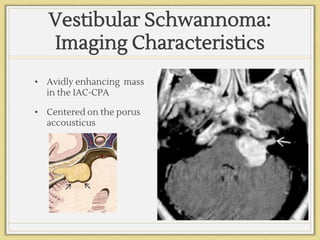
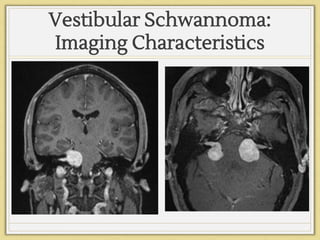
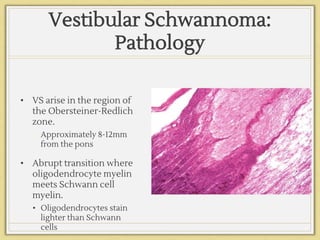
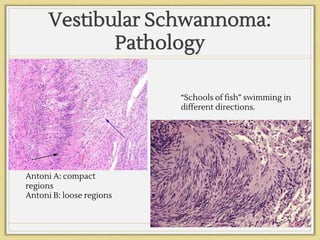
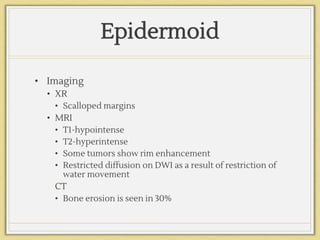
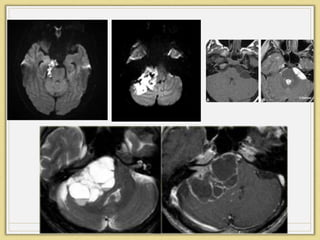
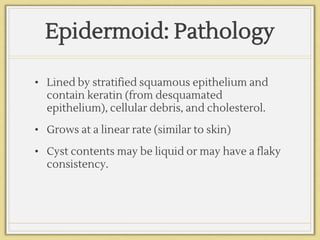
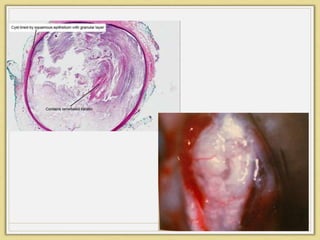
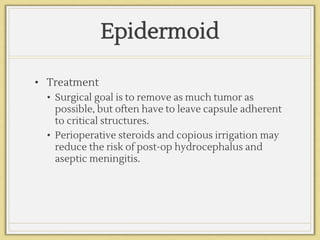
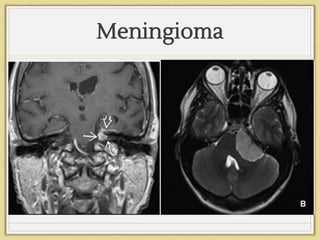
- Common pathologies include vestibular schwannomas, meningiomas, and epidermoids. Vestibular schwannomas are the most common tumor.
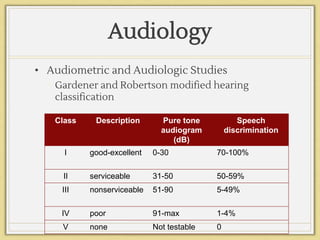
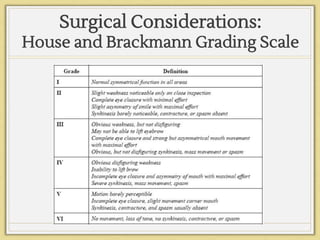
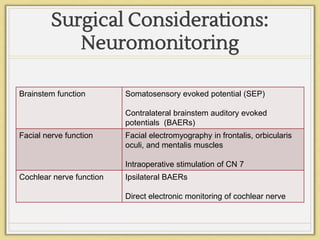
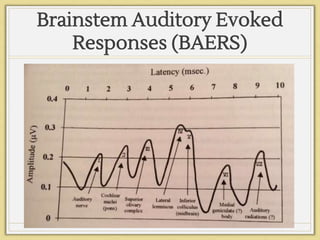
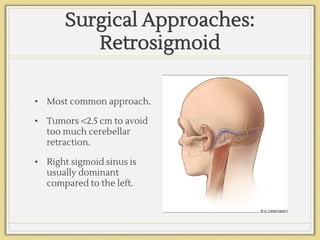
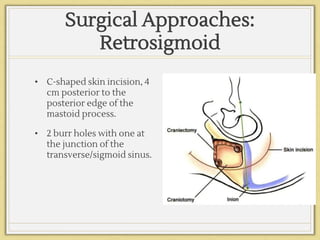
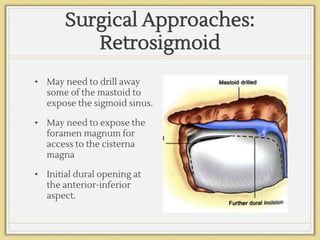
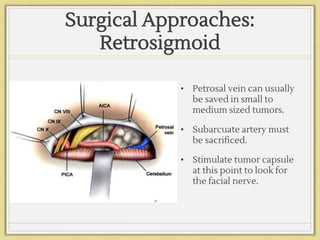
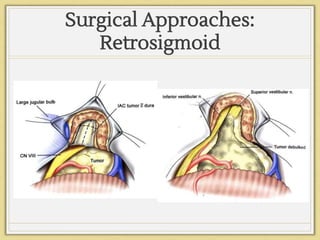
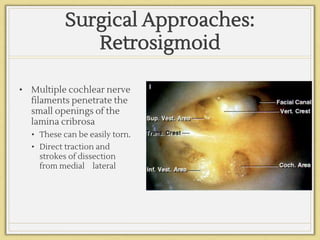
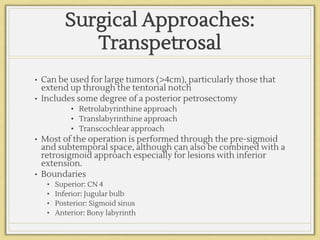
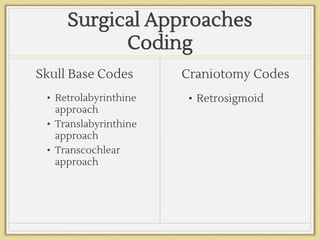
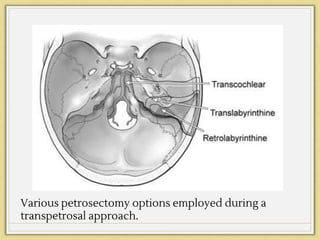
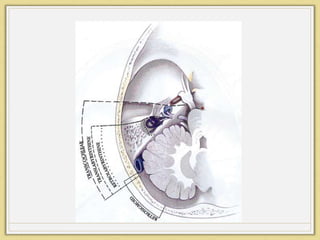
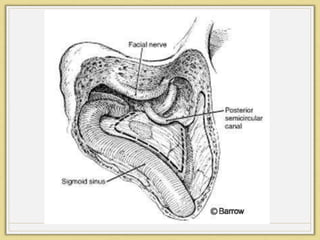
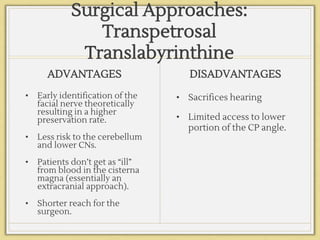
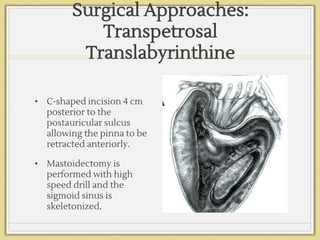
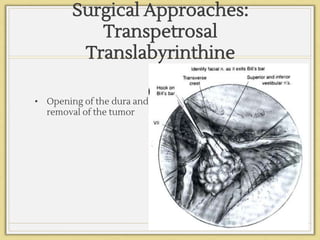
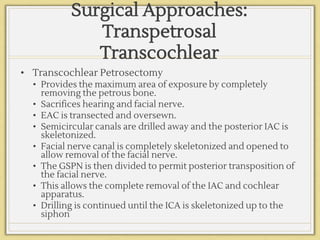
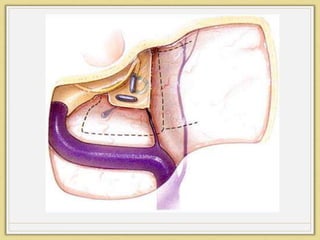
- Surgical approaches aim to remove the tumor while preserving hearing and facial nerve function. The retrosigmoid approach is most common but transpetrosal approaches are used for large tumors.