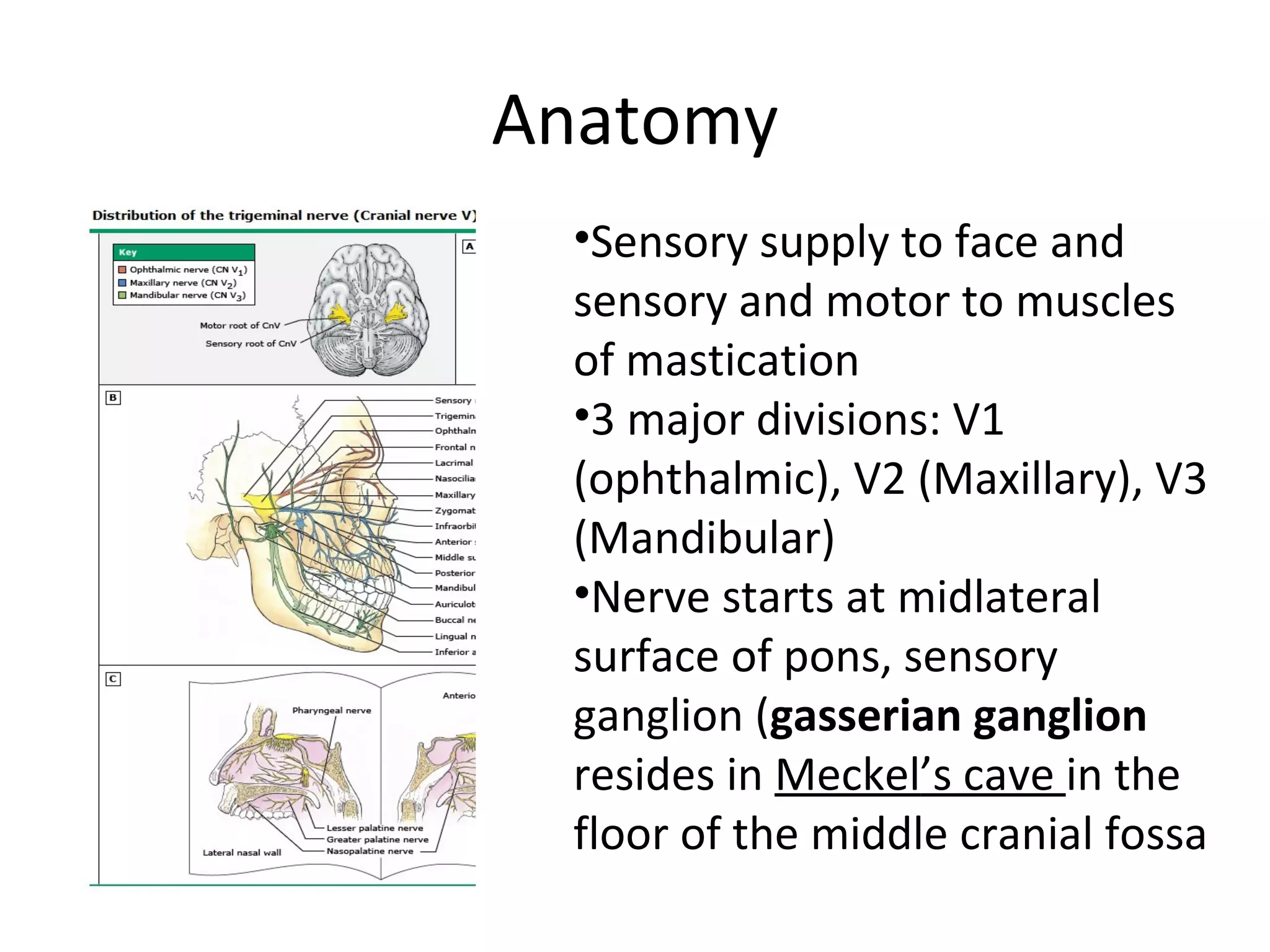
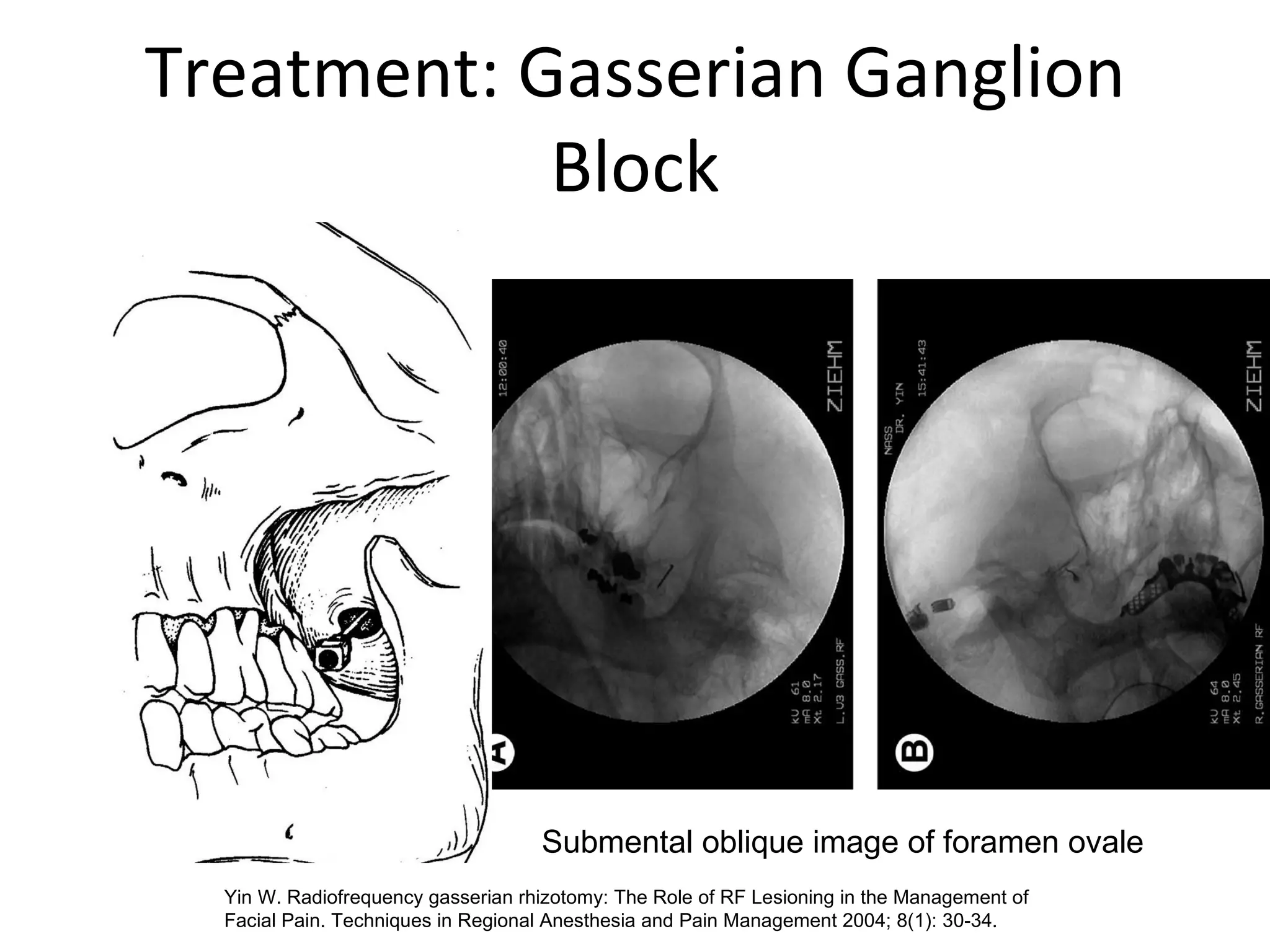
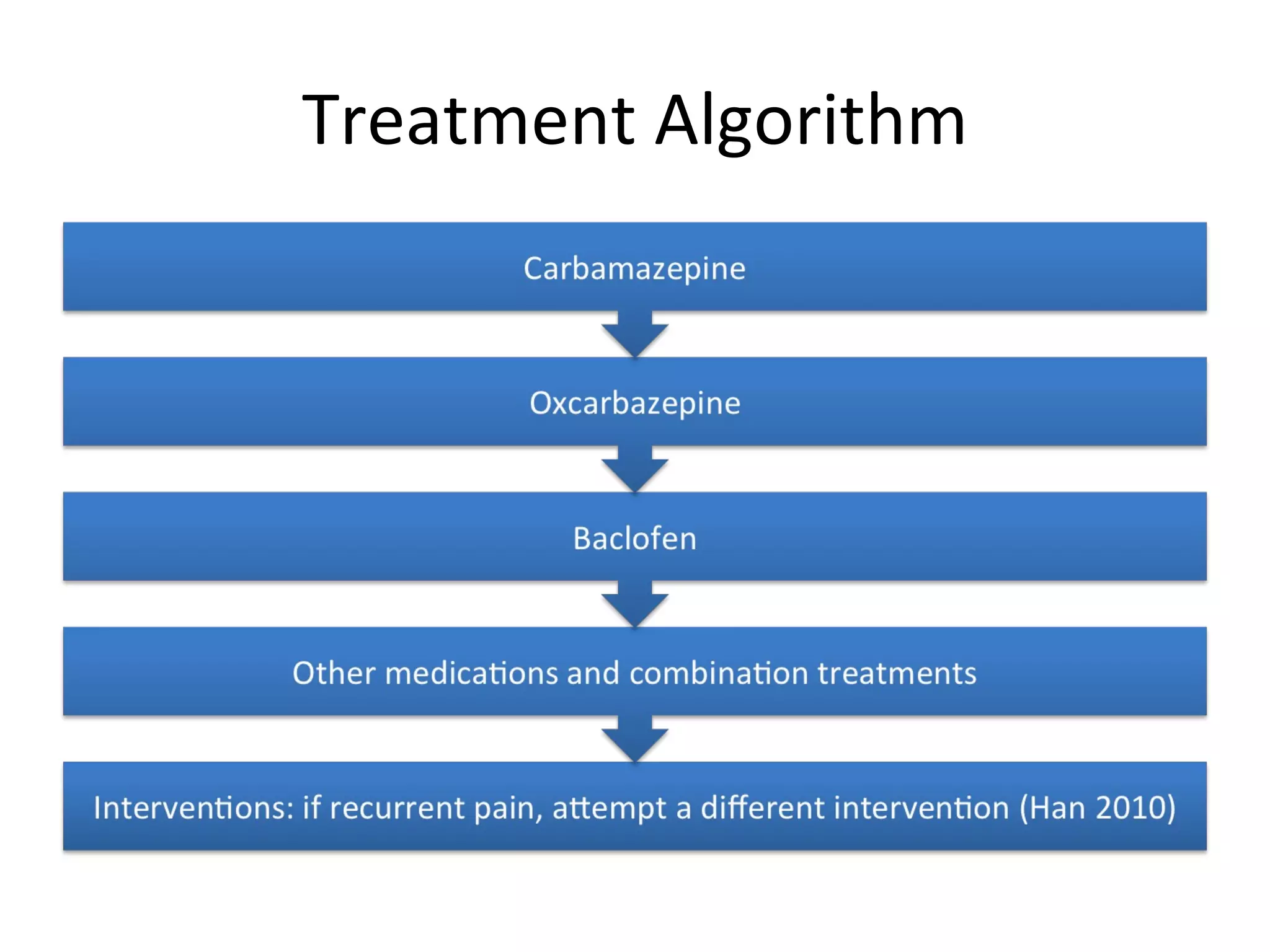
Trigeminal neuralgia is a neuropathic disorder characterized by severe, sporadic facial pain. It is caused most commonly by vascular compression of the trigeminal nerve near the brainstem. Carbamazepine is first-line medical treatment but has side effects. Interventional treatments include microvascular decompression, rhizotomy, and gamma knife radiosurgery which provide initial pain relief in the majority but have risks of sensory deficits. Treatment is aimed at pain control and improving quality of life.