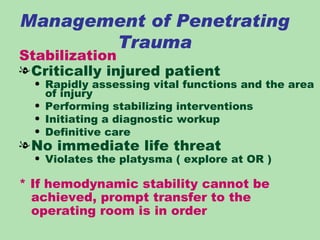
This document discusses the assessment and management of neck trauma, including penetrating trauma, blunt trauma, and strangulation injuries. It covers the pathophysiology, classification, clinical features, diagnostic evaluation and definitive treatment for various types of neck injuries. The management involves a structured approach to stabilize the patient, assess airway and vascular integrity, perform diagnostic studies as needed, and determine whether surgical intervention is required to address injuries from penetrating trauma or signs of injury from blunt trauma.