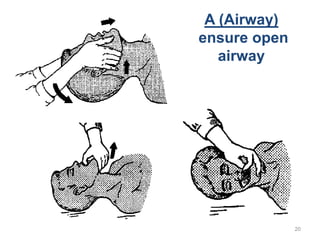
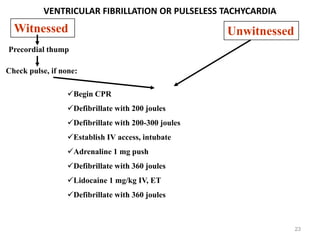
This document provides information on cardiopulmonary resuscitation (CPR) including its history, techniques, terminology, diagnosis of cardiac arrest, and guidelines from the American Heart Association (AHA). It discusses the development of CPR from the 19th century to modern times. The 2010 AHA guidelines emphasize high-quality chest compressions, early defibrillation, and post-cardiac arrest care including therapeutic hypothermia. The guidelines provide updated recommendations for compression rate, depth, ventilation rates, and other aspects of CPR for adults, children, and infants.