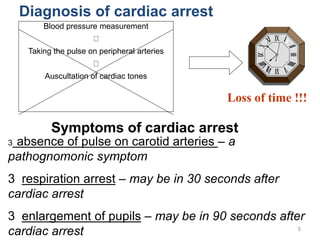
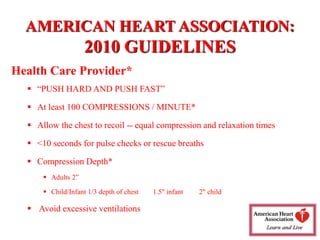
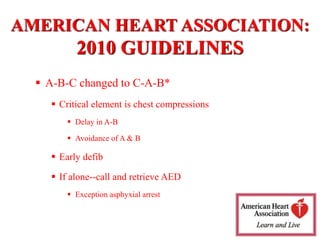
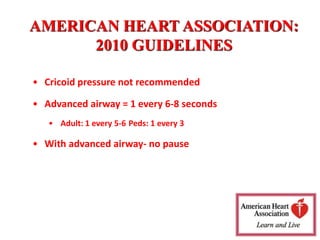
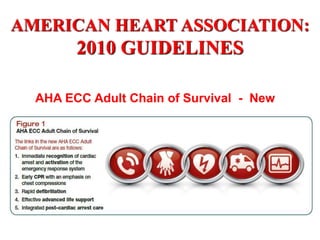
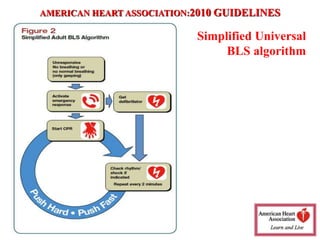
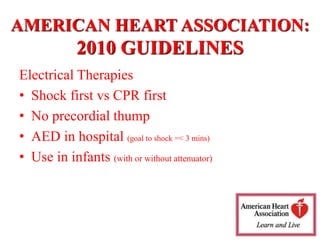
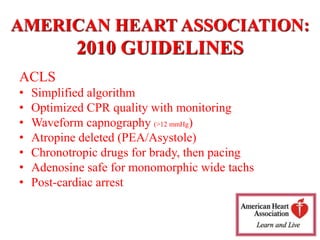
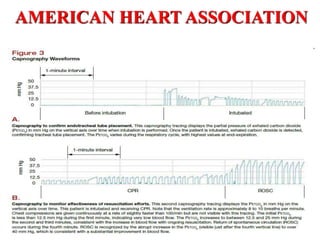
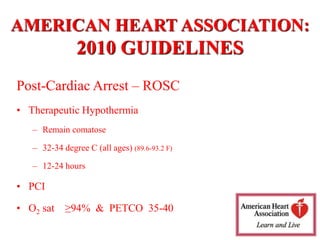
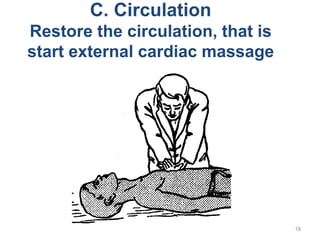
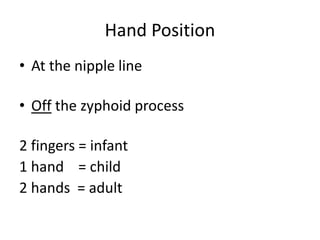
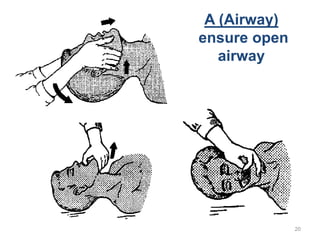
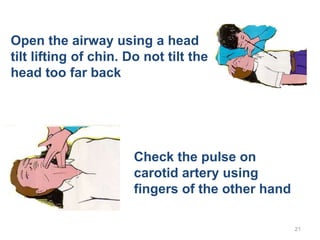
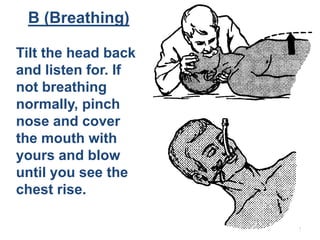
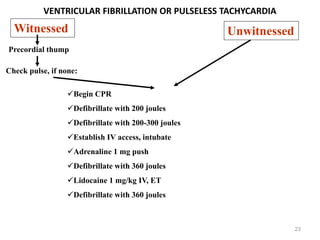
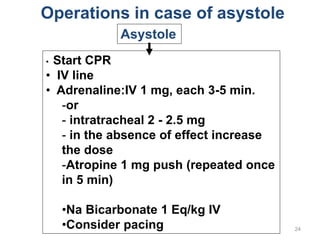
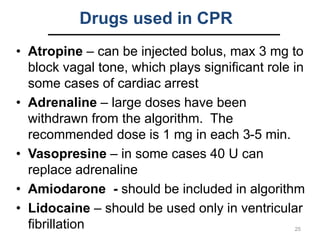
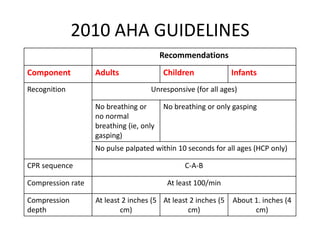
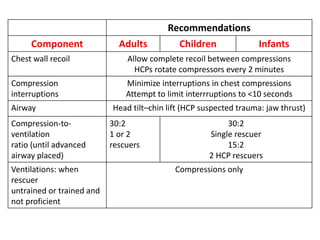
This document provides an overview of the history and guidelines for cardiopulmonary resuscitation (CPR). It discusses the origins and early developments of CPR in the 19th-20th centuries. It then summarizes the key guidelines from the 2010 American Heart Association, including performing chest compressions at a rate of 100 per minute with full chest recoil, minimizing interruptions, and emphasizing compression-only CPR for untrained rescuers. The guidelines are reviewed for different age groups and scenarios. Special resuscitation situations like drowning, hypothermia, and post-cardiac arrest care are also covered.