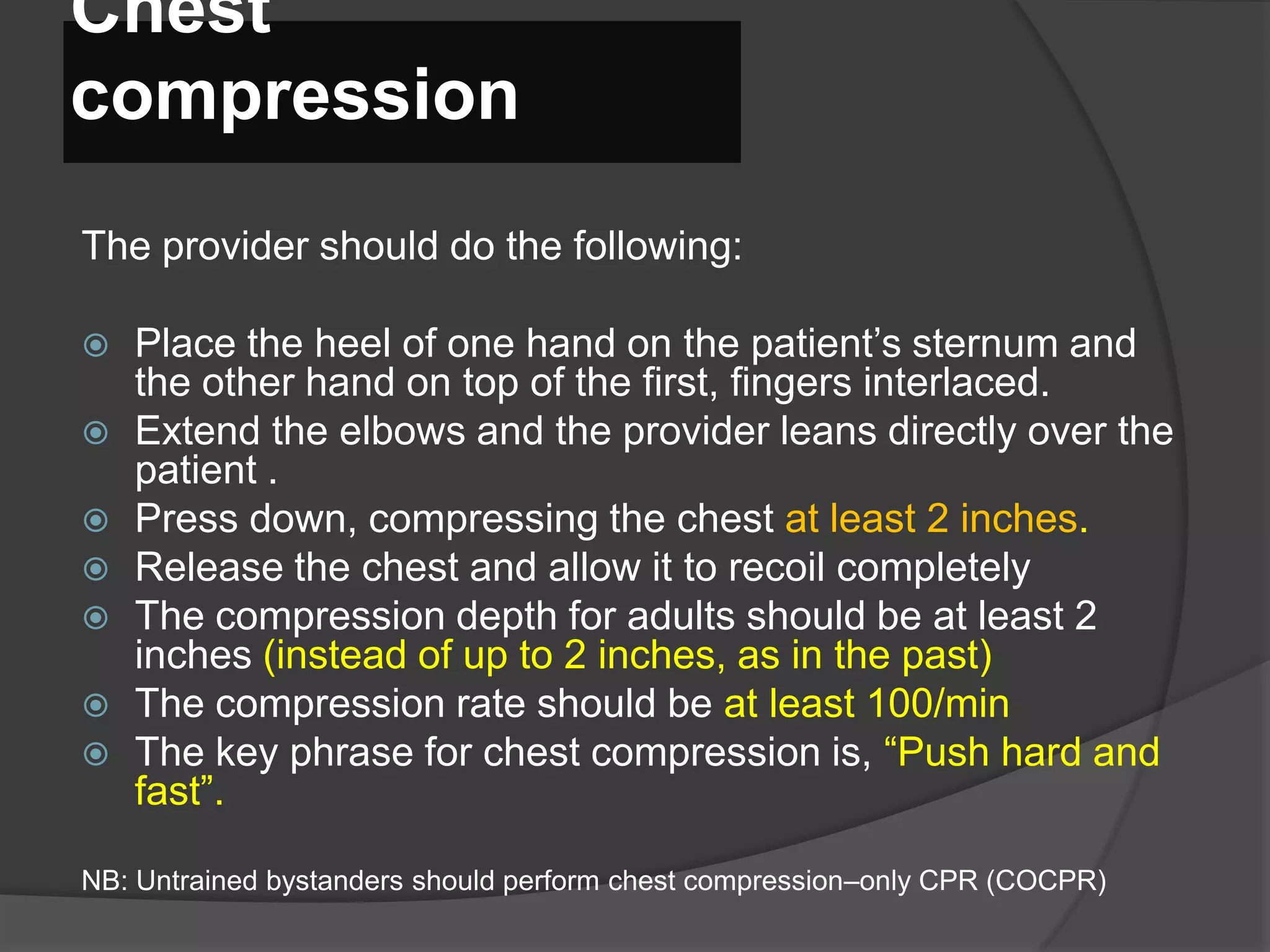
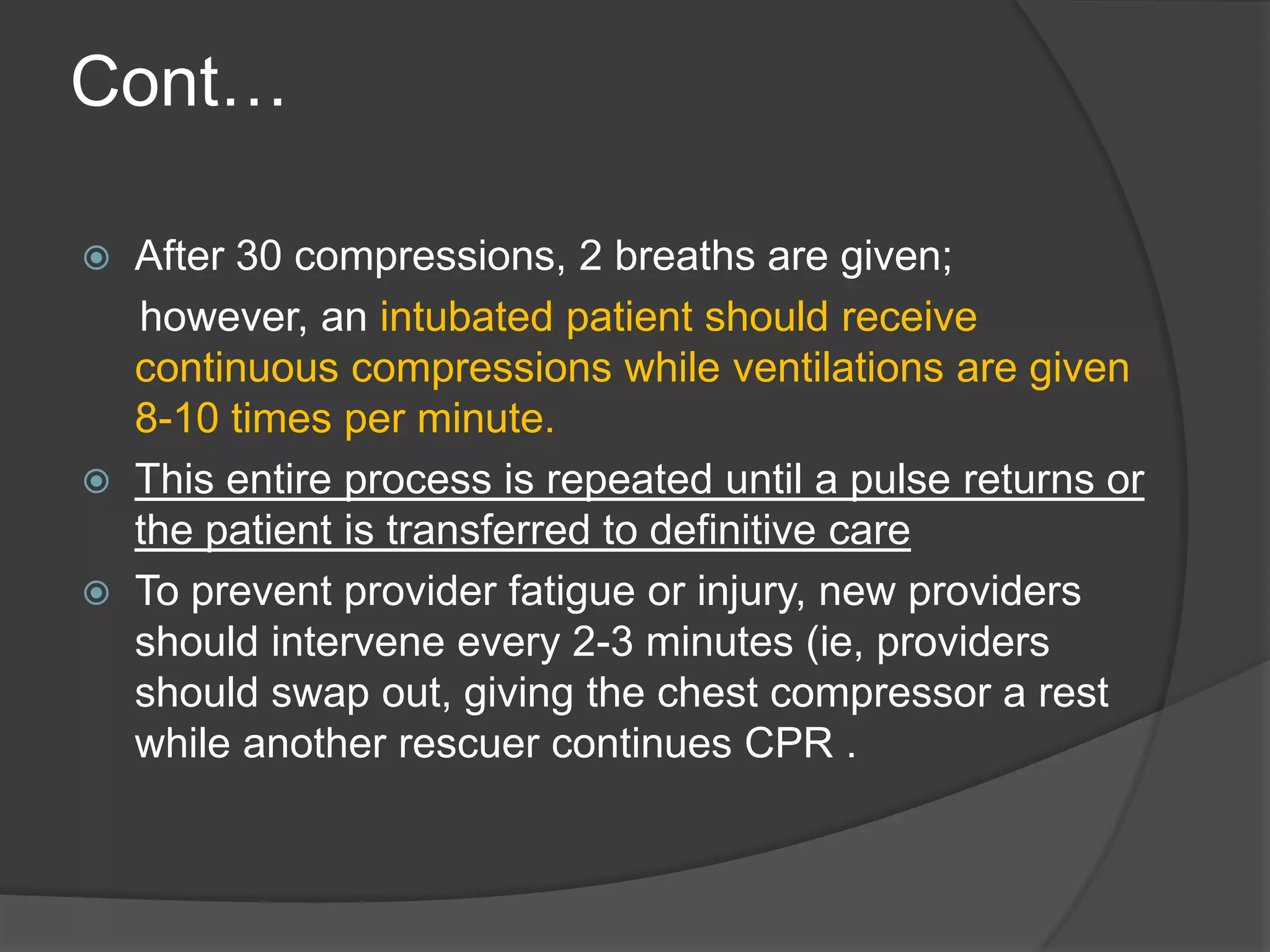
This document discusses cardiopulmonary resuscitation (CPR) techniques and a study that found a combination of vasopressin, steroids, and epinephrine during CPR led to improved outcomes compared to epinephrine alone. It provides details on performing CPR, including chest compressions, ventilation, positioning, and guidelines for adults, children and infants. Videos are referenced to demonstrate CPR and use of an automated external defibrillator. Potential complications of CPR like rib fractures and gastric insufflation are also mentioned.


























![Post-Procedure
Complications:
Performing chest compressions may result in the
fracturing of ribs or the sternum, though the
incidence of such fractures is widely considered to
be low.
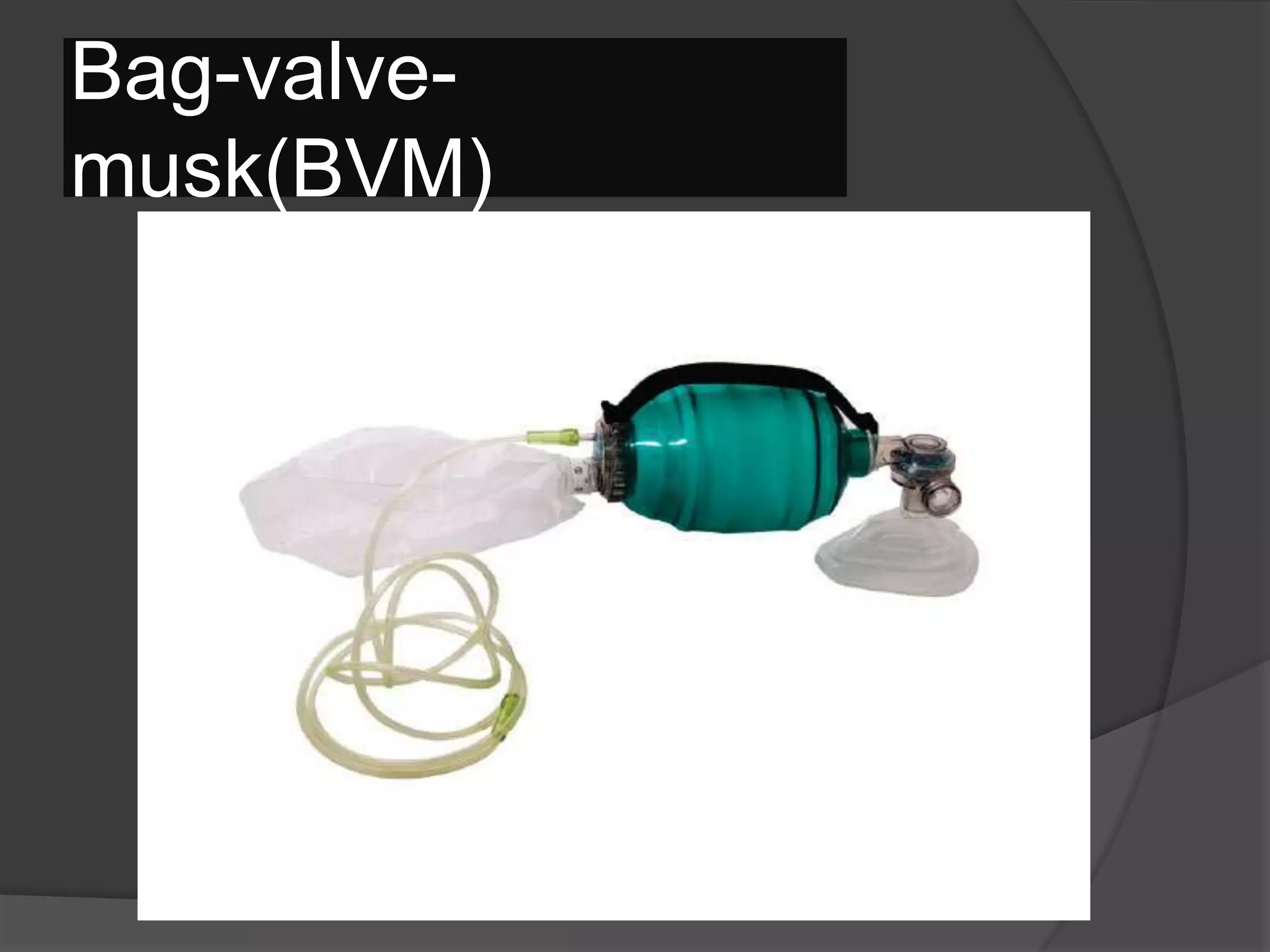
Artificial respiration using noninvasive ventilation
methods (eg, mouth-to-mouth, bag-valve-mask
[BVM]) can often result in gastric insufflation. This
can lead to vomiting, which can further lead to
airway compromise or aspiration. The problem is
eliminated by inserting an invasive airway, which
prevents air from entering the esophagus.](https://image.slidesharecdn.com/cardiopulmonaryresuscitationcpr-140520061340-phpapp02/75/Cardiopulmonary-resuscitation-cpr-40-2048.jpg)
