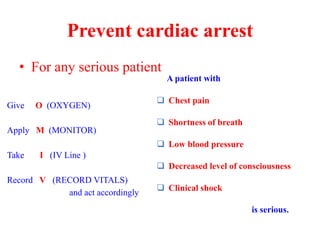
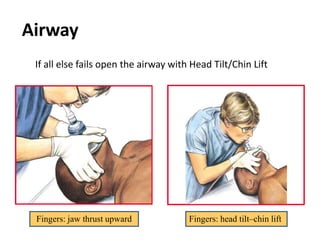
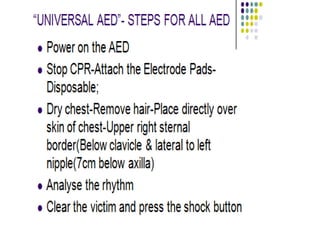
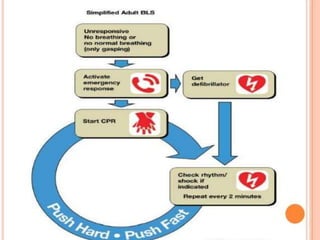
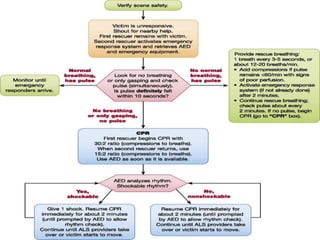
The document outlines the essential protocols for Basic Life Support (BLS) and the AHA Chains of Survival for adult cardiac arrest management, emphasizing prompt intervention. It details the importance of immediate CPR, the common causes of cardiac arrest, and provides guidelines on performing chest compressions, clearing the airway, and administering rescue breaths. Additionally, it highlights the significance of teamwork, bystander CPR, and the use of Automated External Defibrillators (AEDs) in emergency situations.