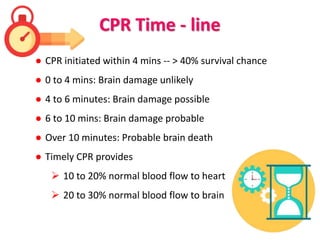
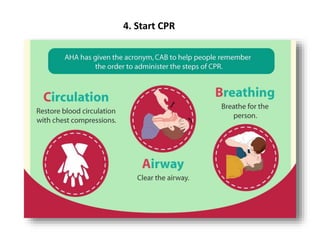
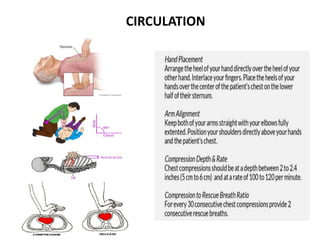
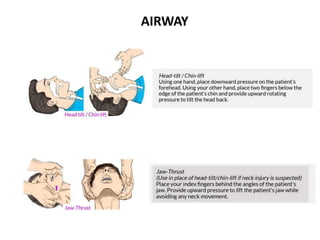
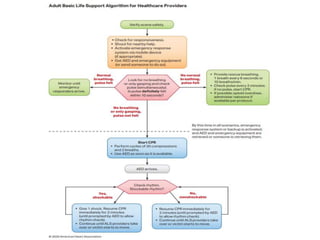
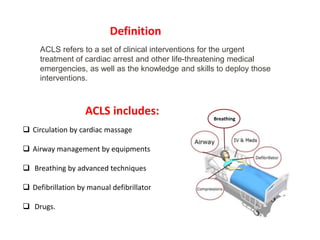
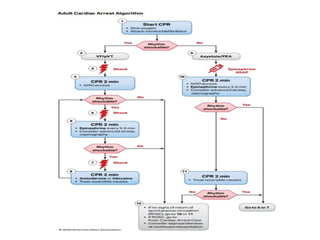
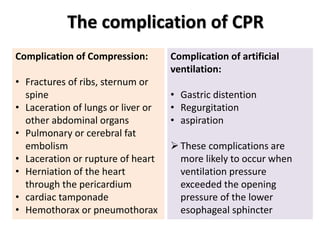
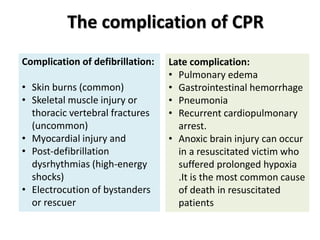
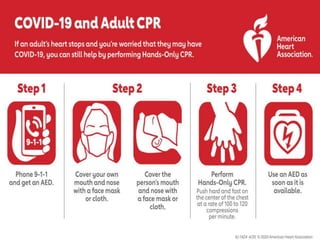
Cardiopulmonary resuscitation (CPR) is an emergency procedure performed when a person's breathing or heartbeat has stopped. CPR involves chest compressions to manually pump blood to vital organs and artificial ventilation to oxygenate the blood. Proper CPR can double or triple a victim's chance of survival after cardiac arrest. The procedure establishes basic circulation and airway support until more advanced medical help arrives.