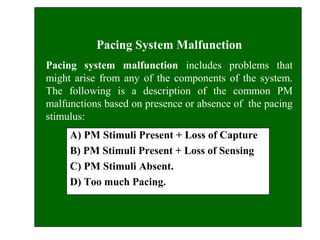
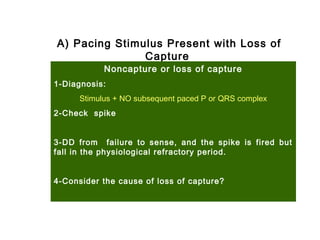
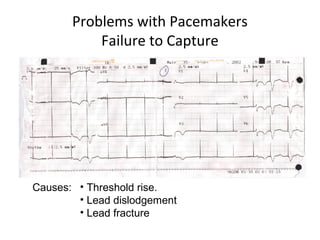
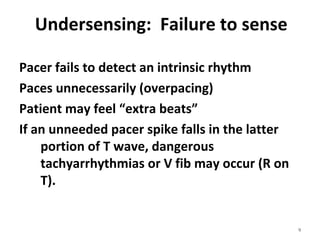
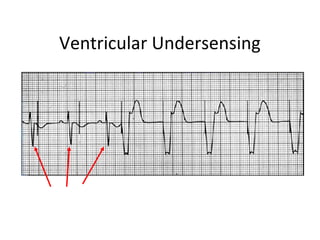
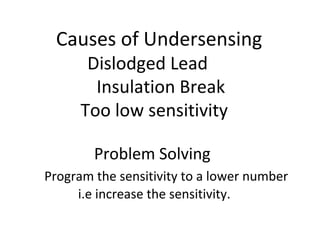
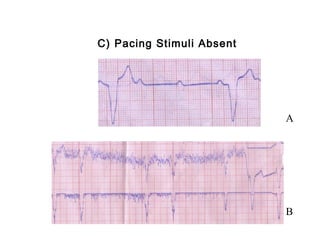
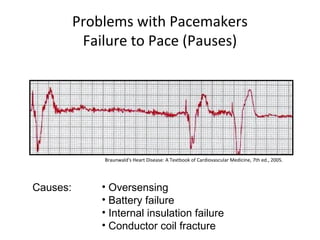
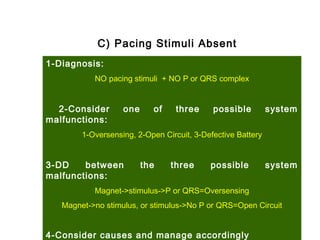
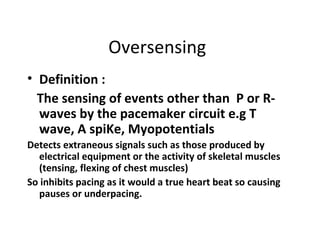
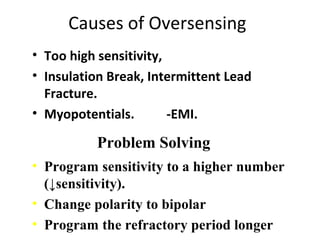
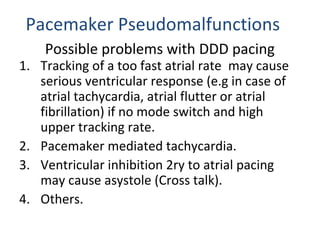
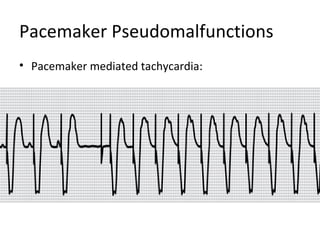
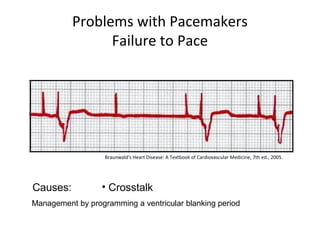
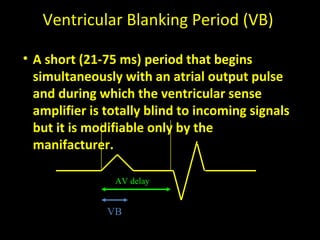
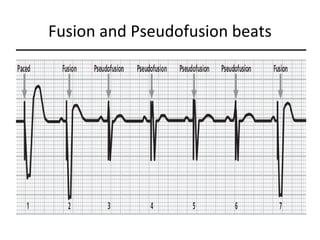
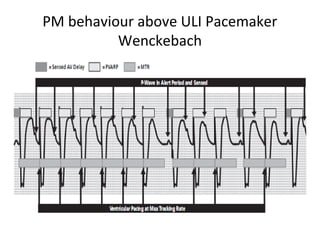
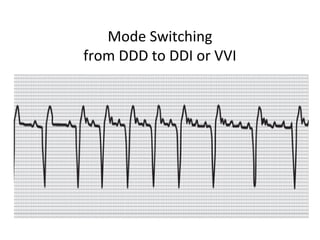
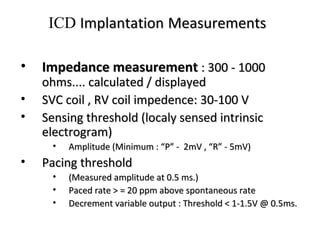
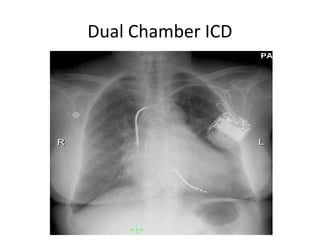
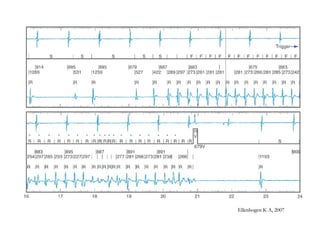
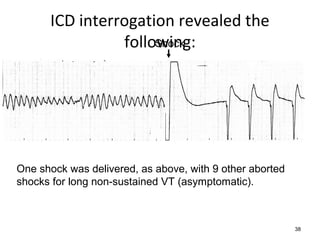
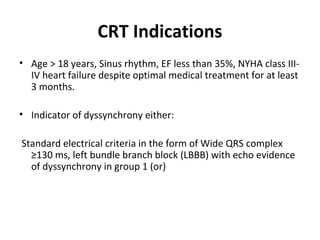
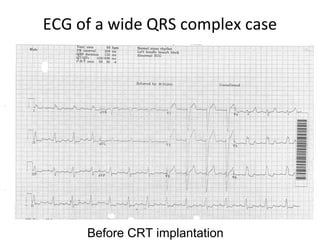
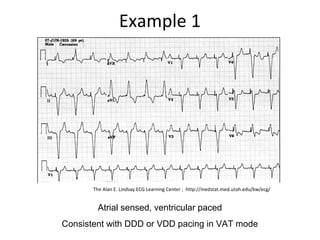
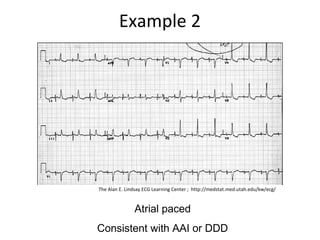
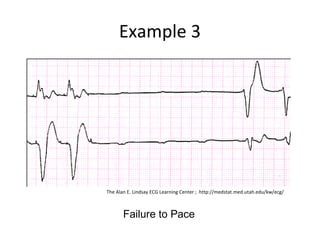
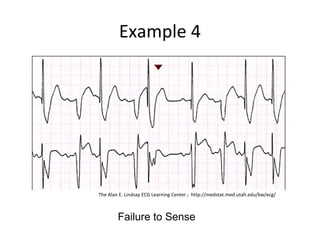
This document discusses potential problems with cardiac pacemakers that are identifiable on ECGs. It describes five main categories of issues: noncapture, undersensing, oversensing, no output, and pseudomalfunctions. Specific problems are then discussed in more detail, including loss of capture, undersensing, absence of pacing stimuli, and overpacing. Causes and diagnostic approaches for each problem are provided. The document also briefly discusses implantable cardioverter defibrillators and cardiac resynchronization therapy.