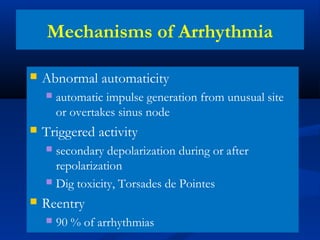
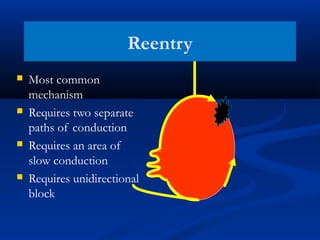
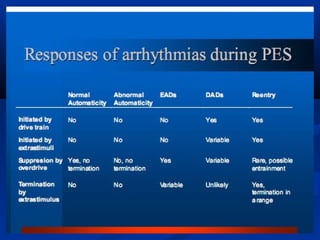
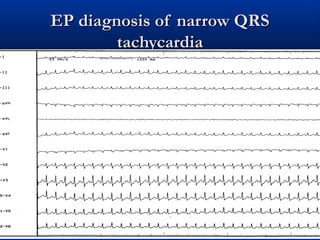
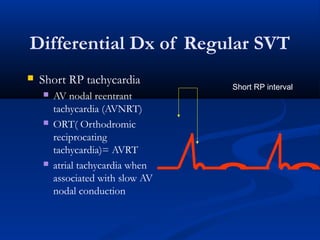
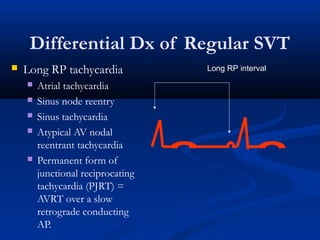
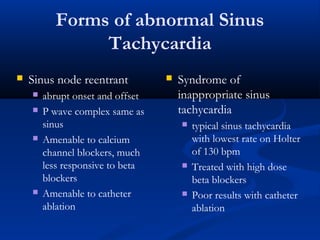
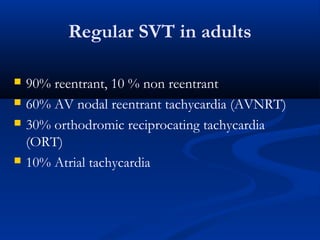
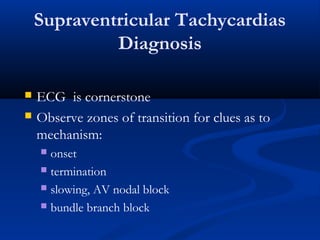
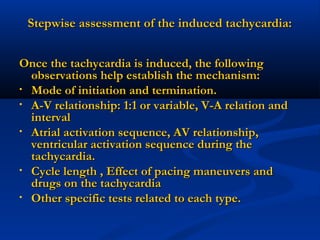
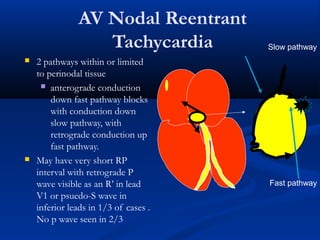
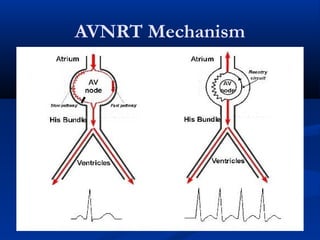
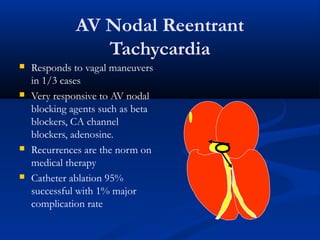
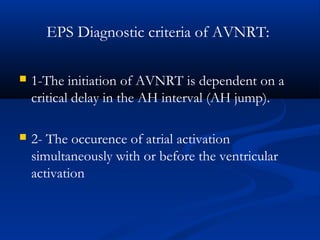
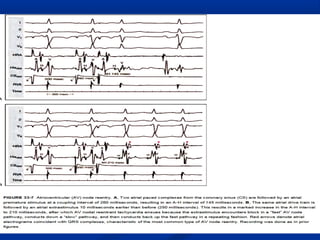
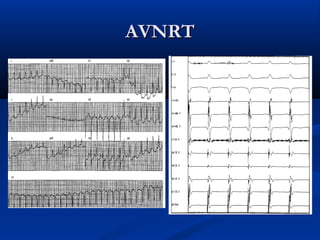
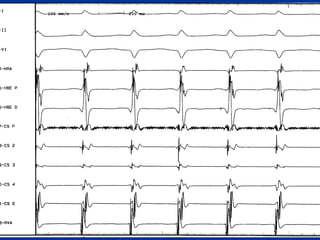
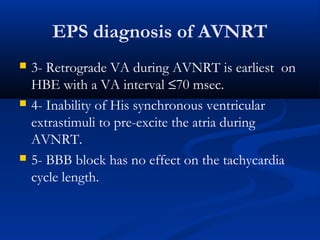
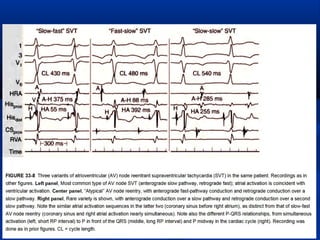
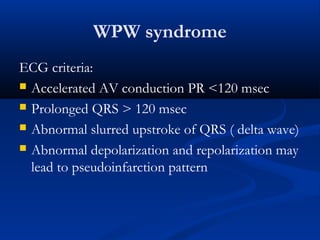
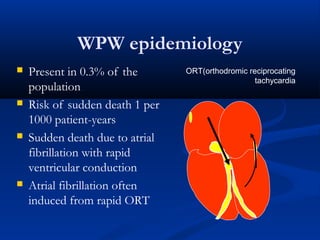
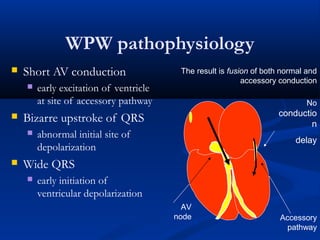
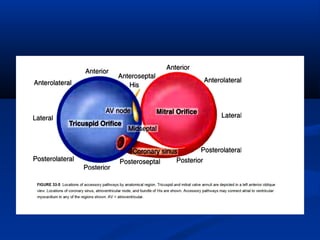
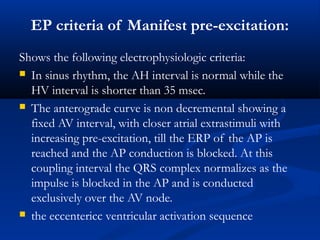
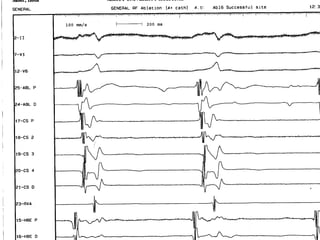
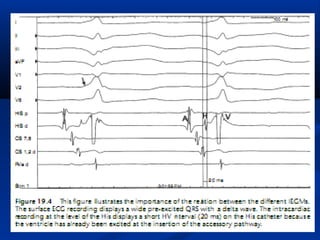
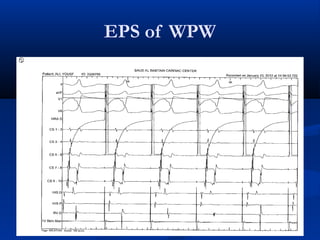
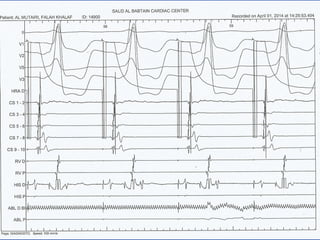
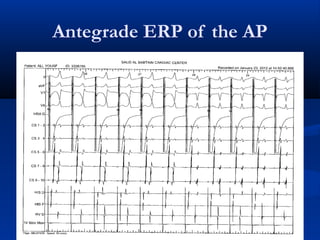
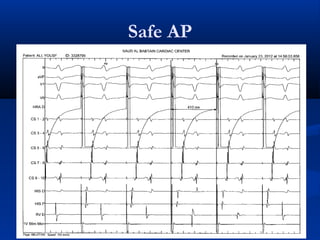
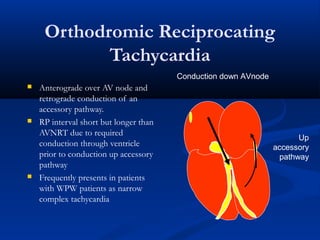
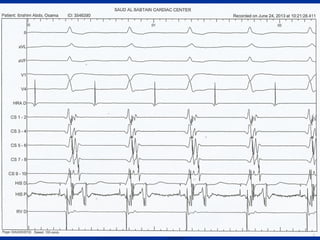
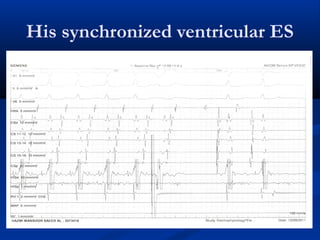
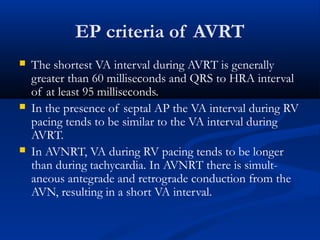
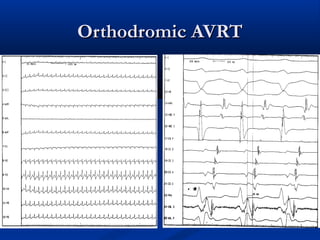
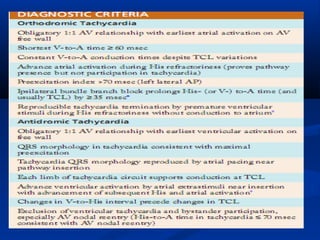
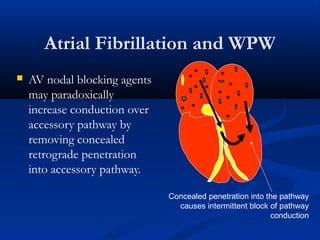
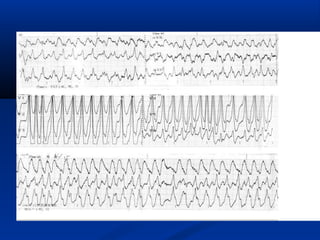
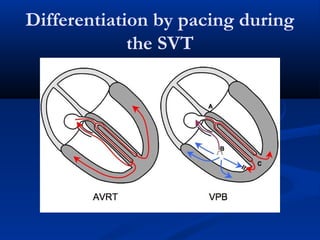
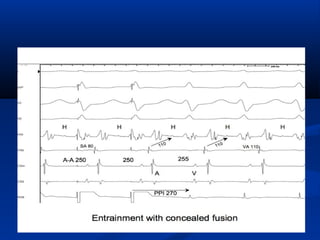
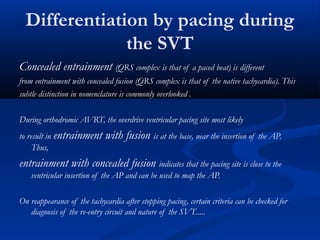
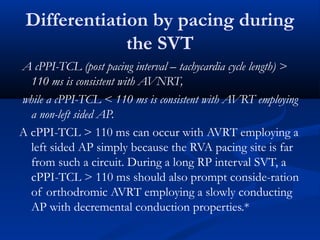
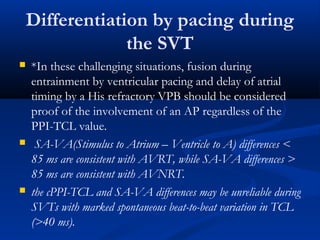
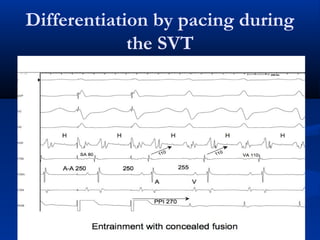
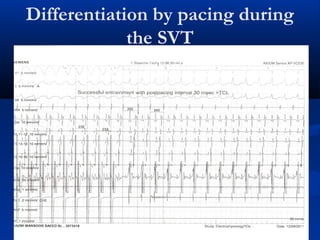
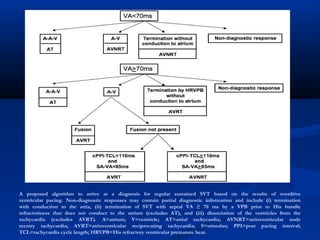
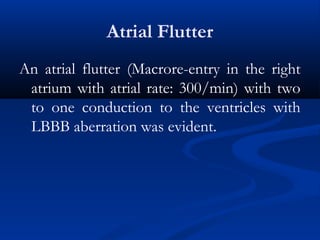
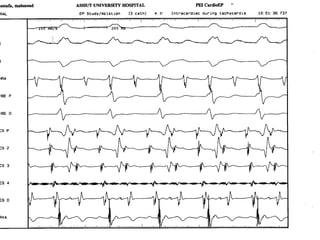
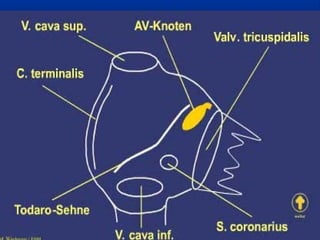
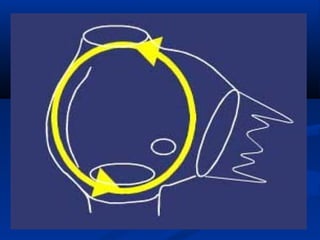
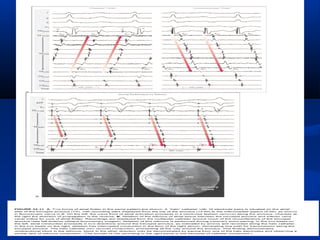
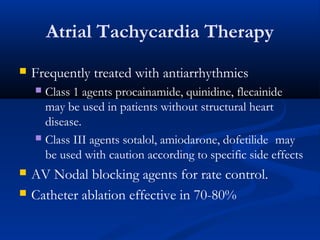
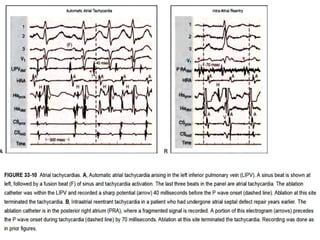
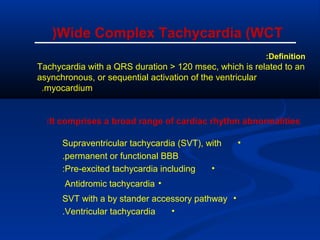
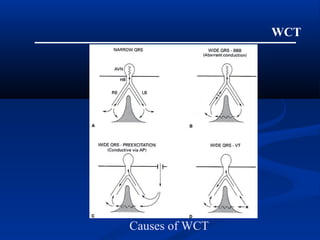
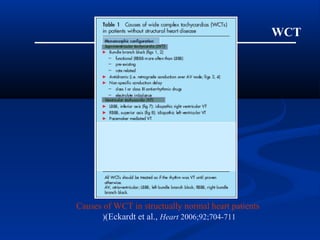
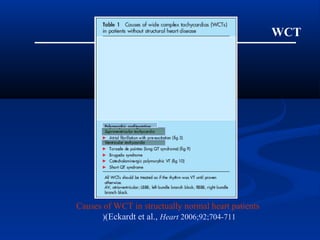
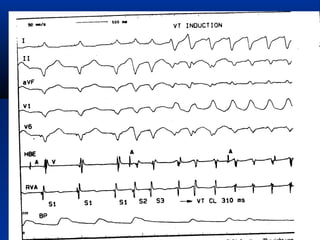
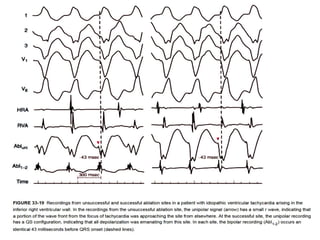
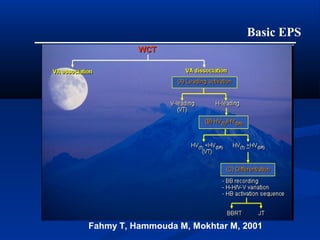
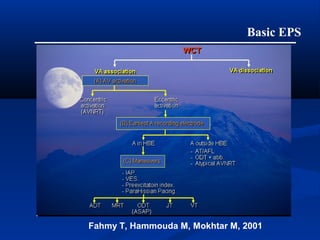
This document discusses various types of arrhythmias including their mechanisms, diagnosis using electrophysiologic studies, and management. It covers topics such as AV nodal reentrant tachycardia, orthodromic reciprocating tachycardia, atrial flutter, atrial tachycardia, Wolff-Parkinson-White syndrome, and differentiation of arrhythmias using pacing techniques during electrophysiology studies. The role of EPS in establishing mechanisms of arrhythmias and guiding treatment is emphasized.