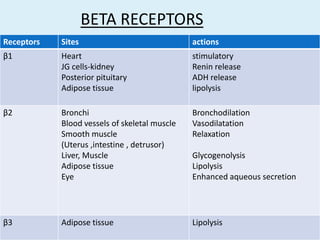
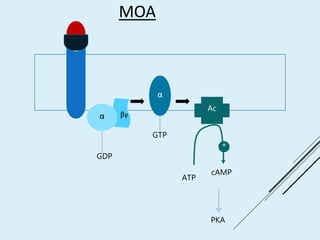
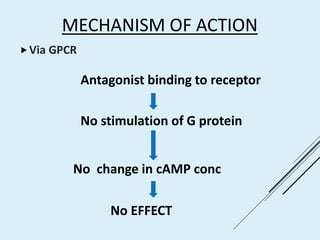
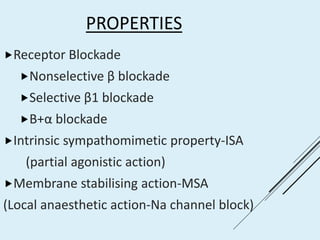
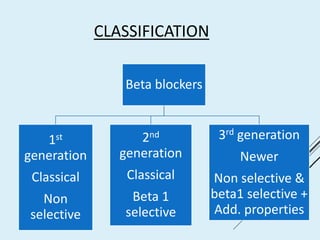
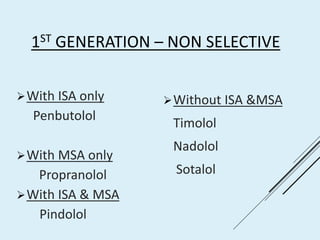
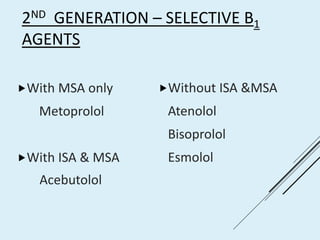
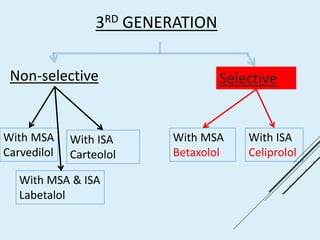
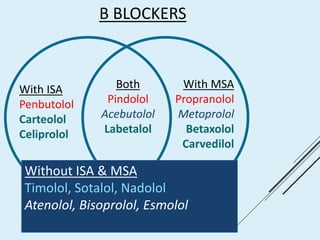
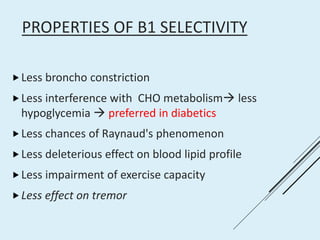
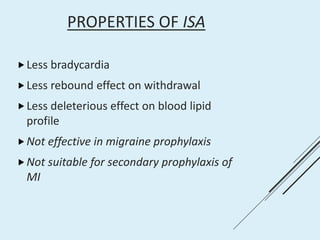
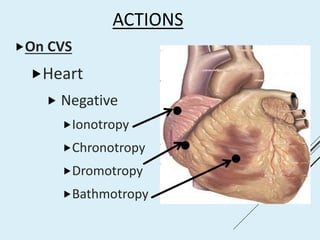
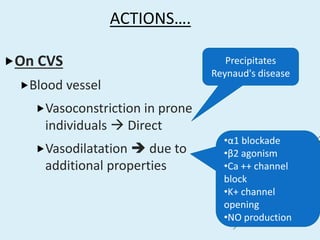
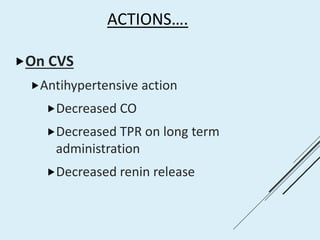
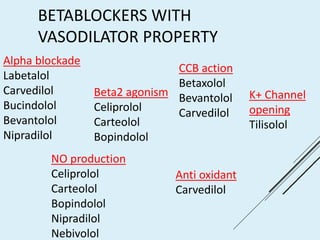
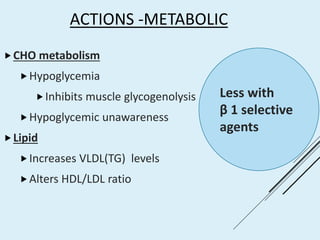
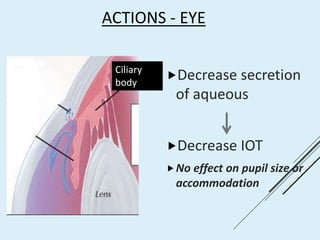
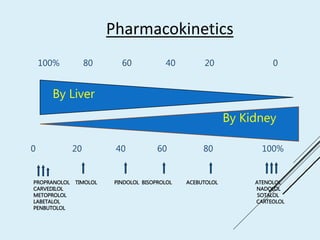
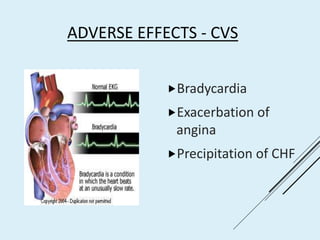
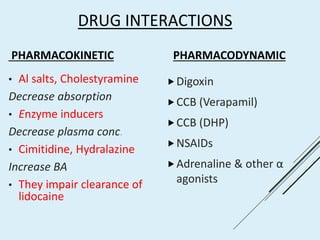
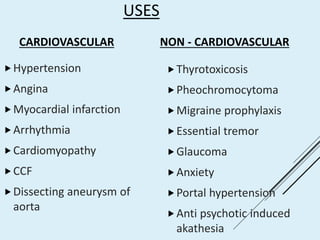
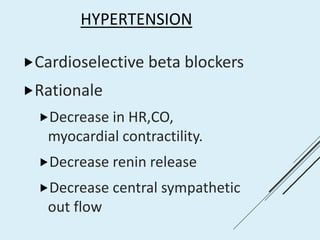
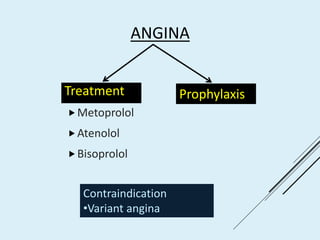
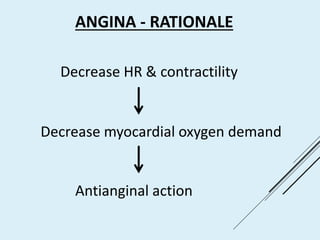
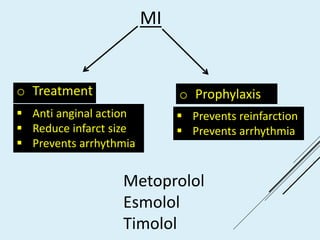
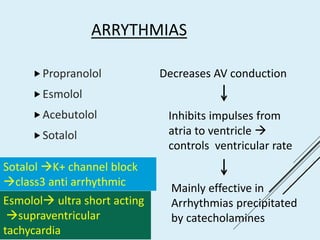
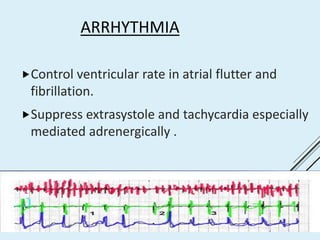
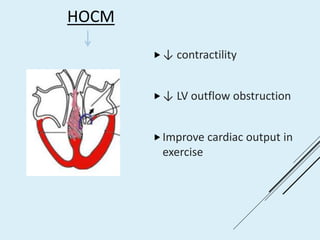
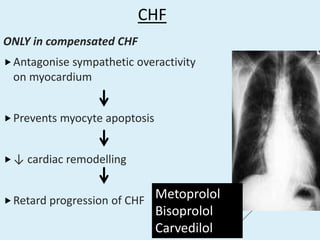
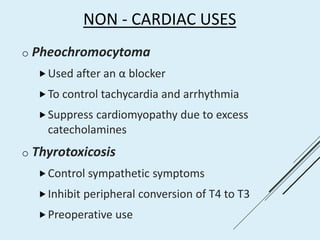
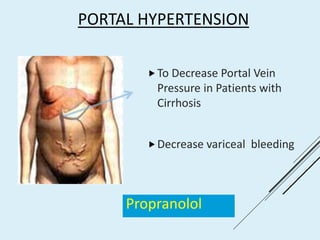
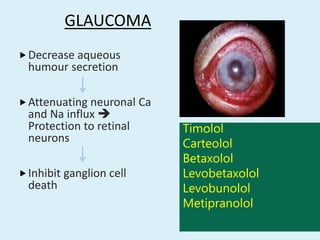
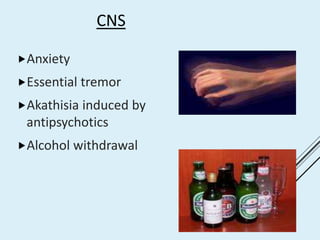
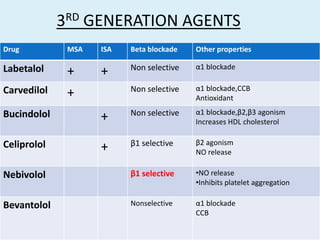
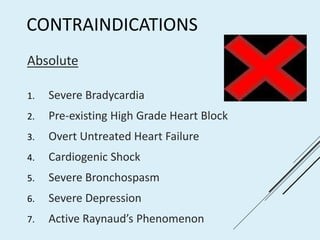
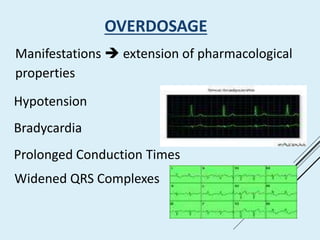
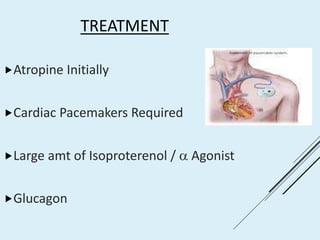
This document summarizes beta blockers, including their mechanism of action, classification, properties, uses, adverse effects and drug interactions. Beta blockers work by blocking beta receptors and inhibiting the adrenergic response. They are classified as first, second or third generation, and can be selective for beta 1 receptors or non-selective. Common uses include hypertension, angina, arrhythmias, migraine prophylaxis and anxiety. Side effects include bradycardia, bronchospasm and hypoglycemia. Drug interactions can occur pharmacokinetically or pharmacodynamically with drugs like digoxin. Overdose treatment involves atropine, pacing and glucagon administration.