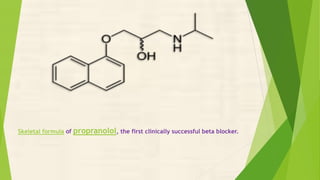
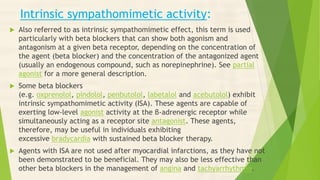
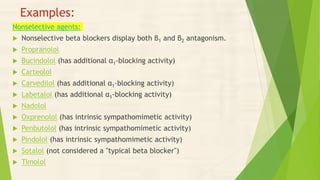
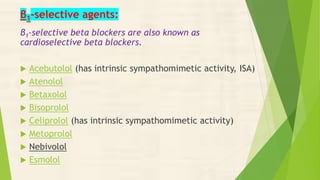
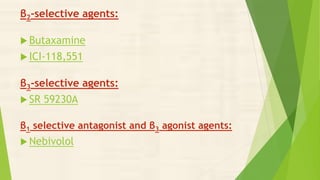
The presentation covers beta blockers, classifying them as competitive antagonists that block adrenergic beta receptors to treat cardiovascular diseases and various other conditions. The origins of beta blockers, their medical uses, mechanisms of action, adverse effects, contraindications, and specific types such as non-selective and beta-1 selective agents are discussed. Additionally, the presentation highlights the performance-enhancing use of beta blockers in sports and the monitoring required during their use.