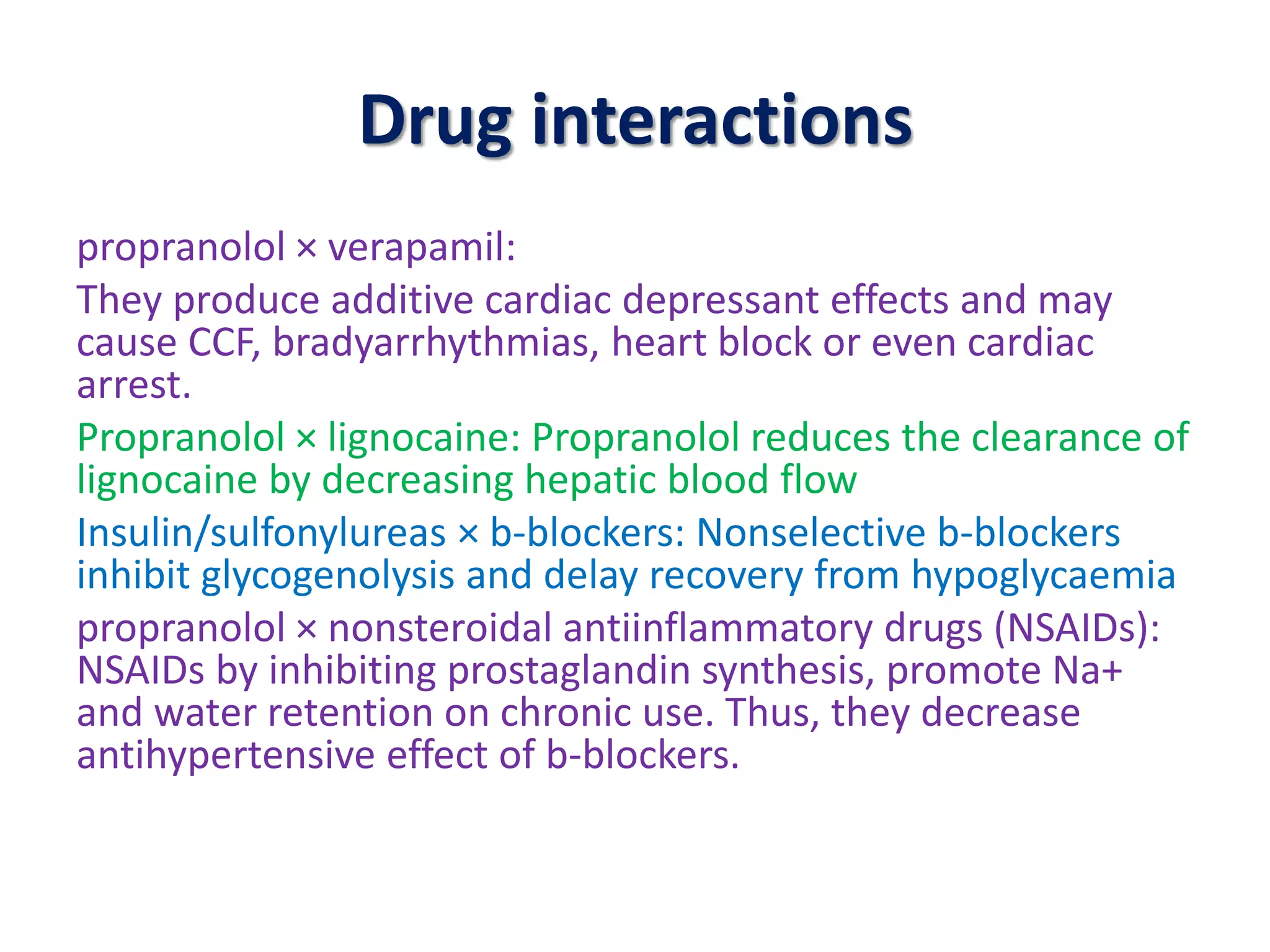
The document discusses the pharmacology and uses of beta blockers, which are drugs that competitively block beta adrenergic receptors to manage cardiovascular conditions. It details their effects on the heart, blood vessels, and respiratory system, highlighting potential adverse effects and drug interactions. Key uses include treating hypertension, angina, myocardial infarction, and other conditions, while cautioning against their use in asthma and respiratory issues.