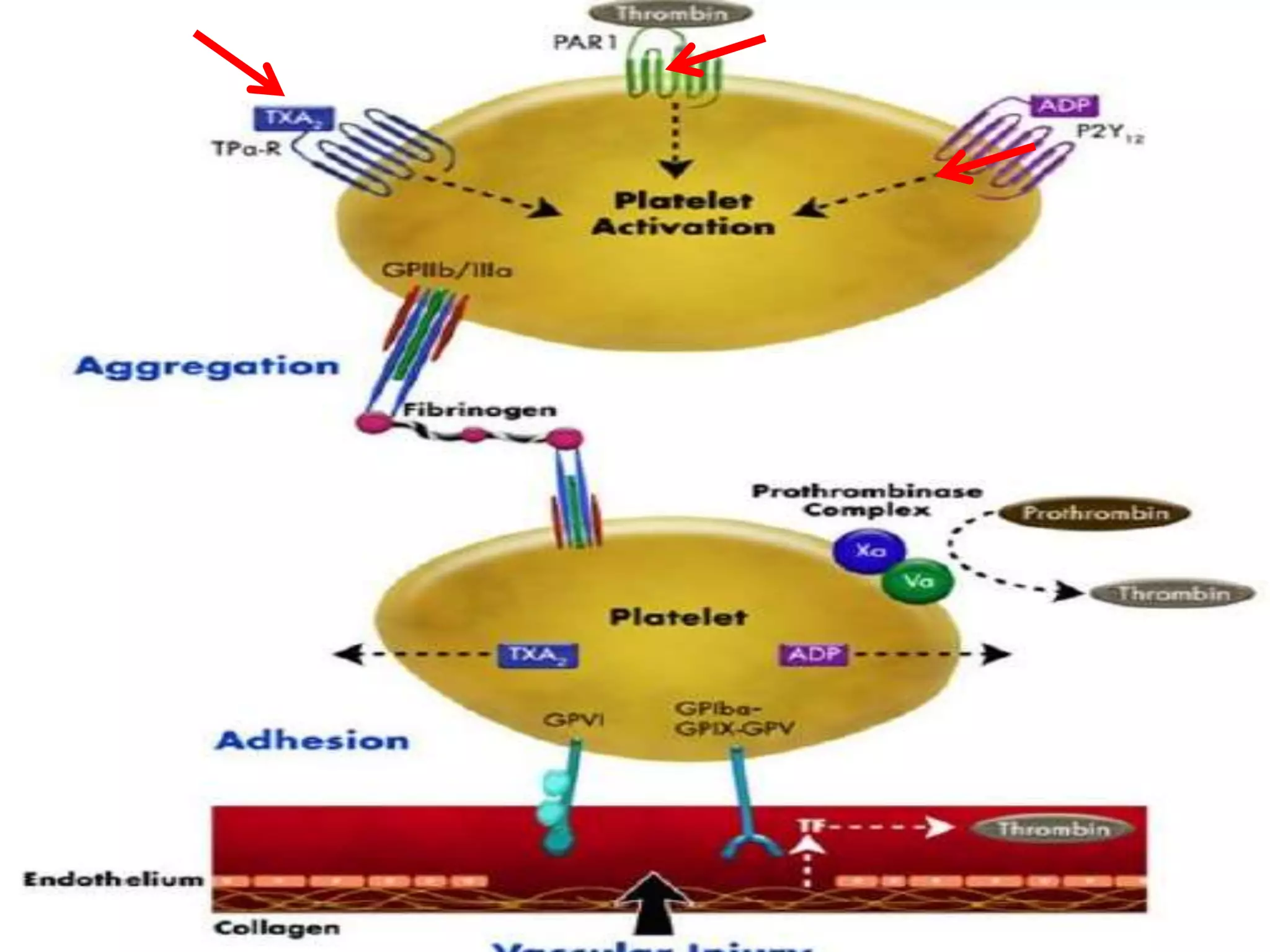
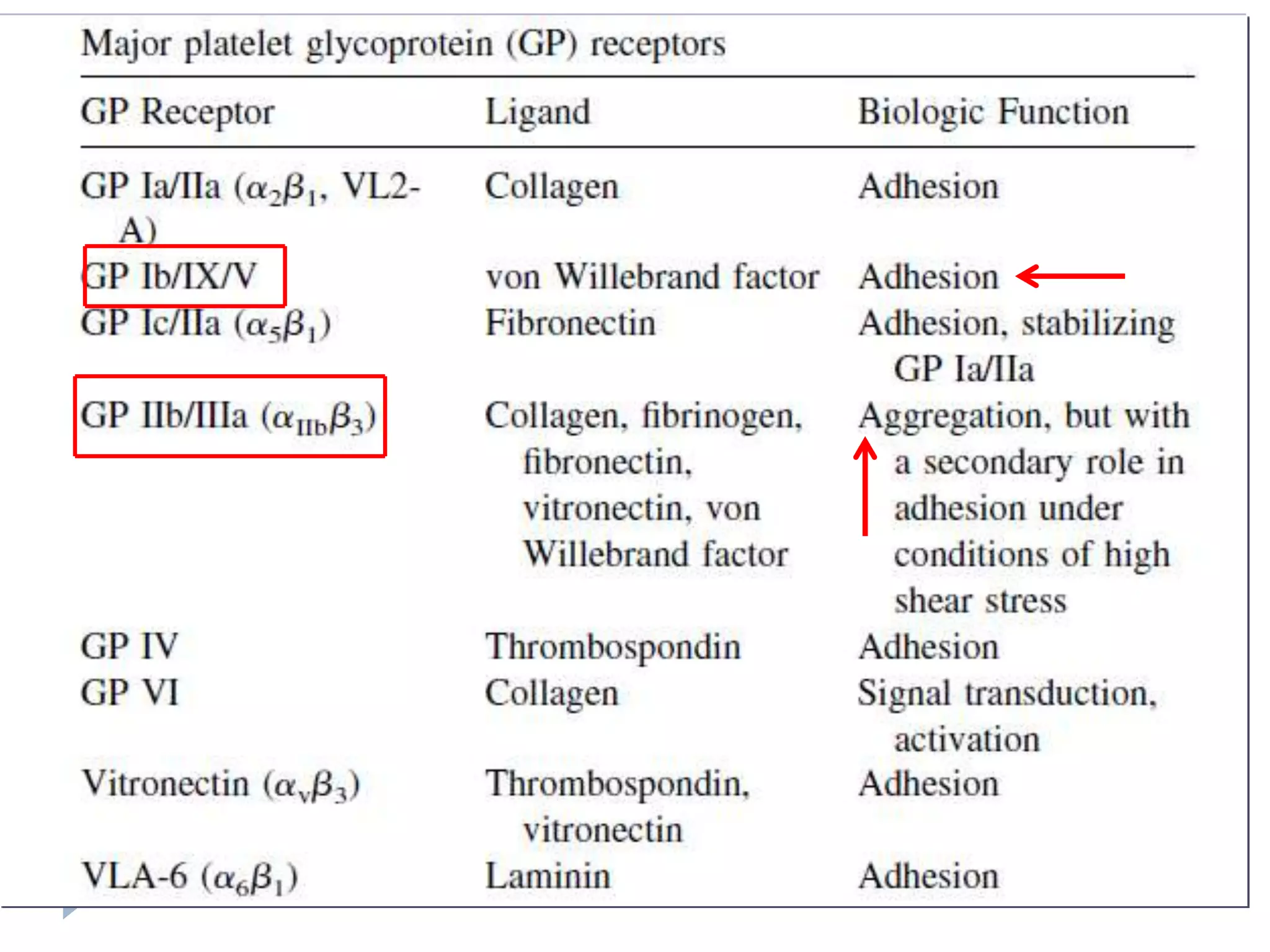
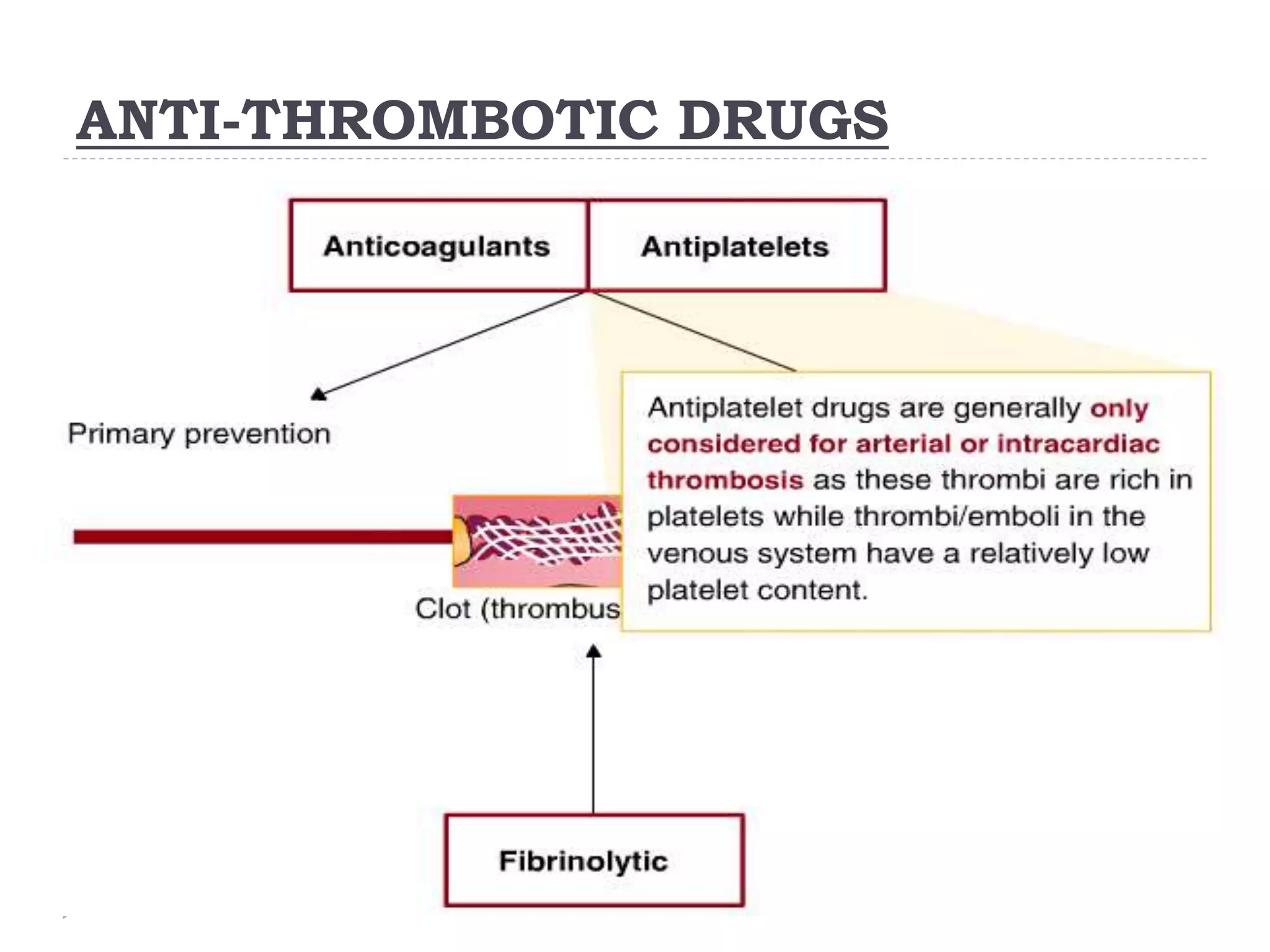
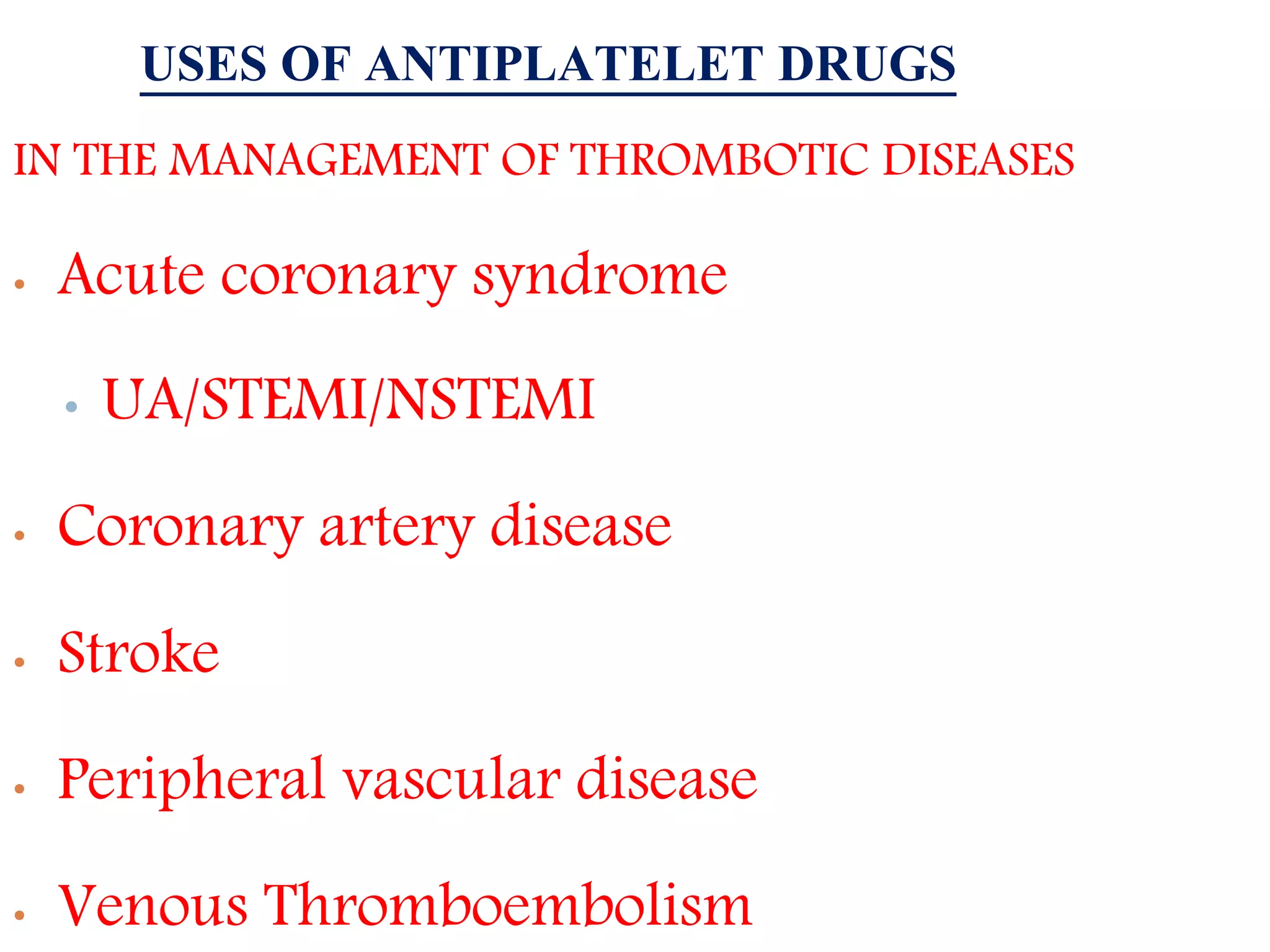
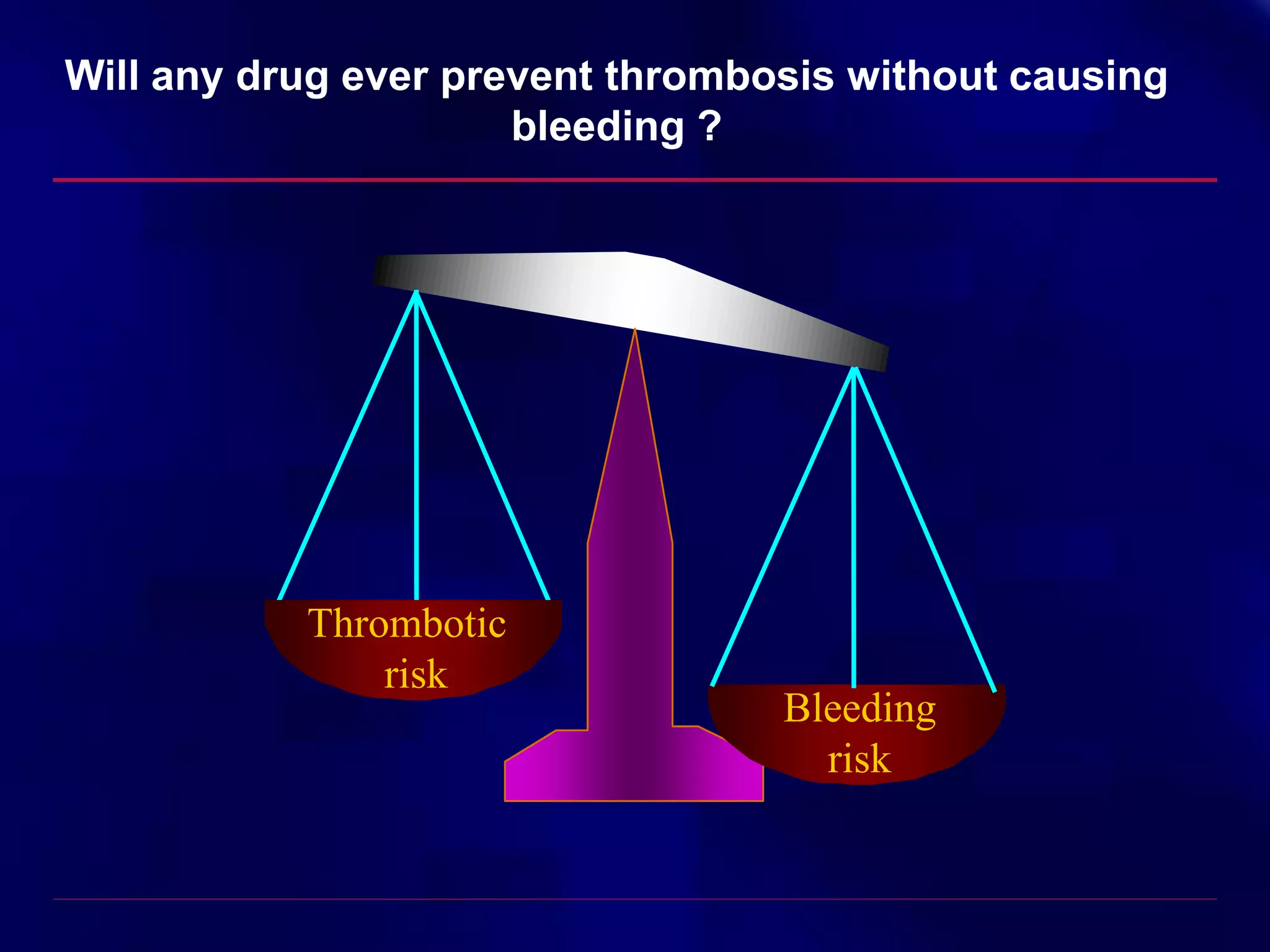
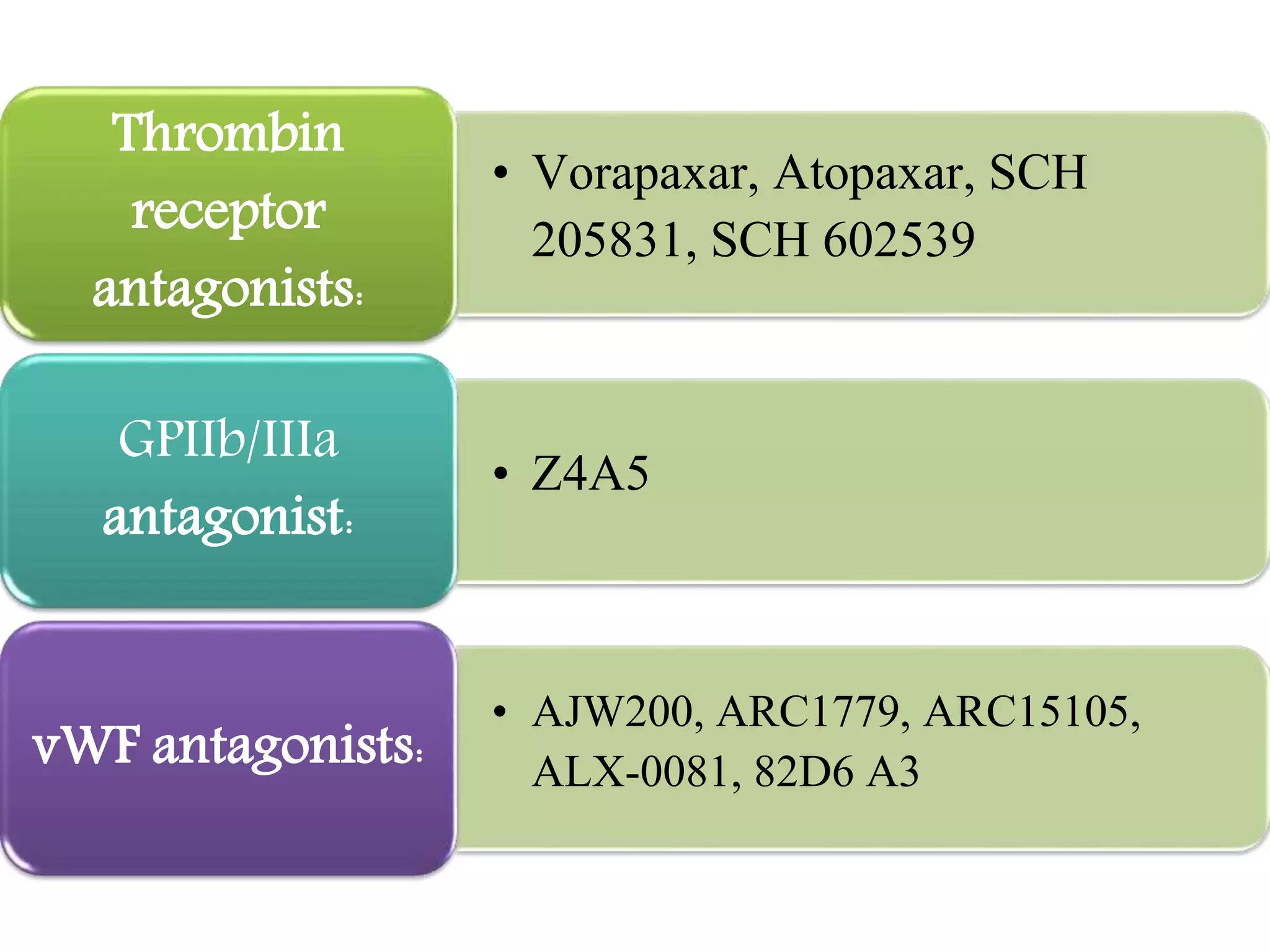
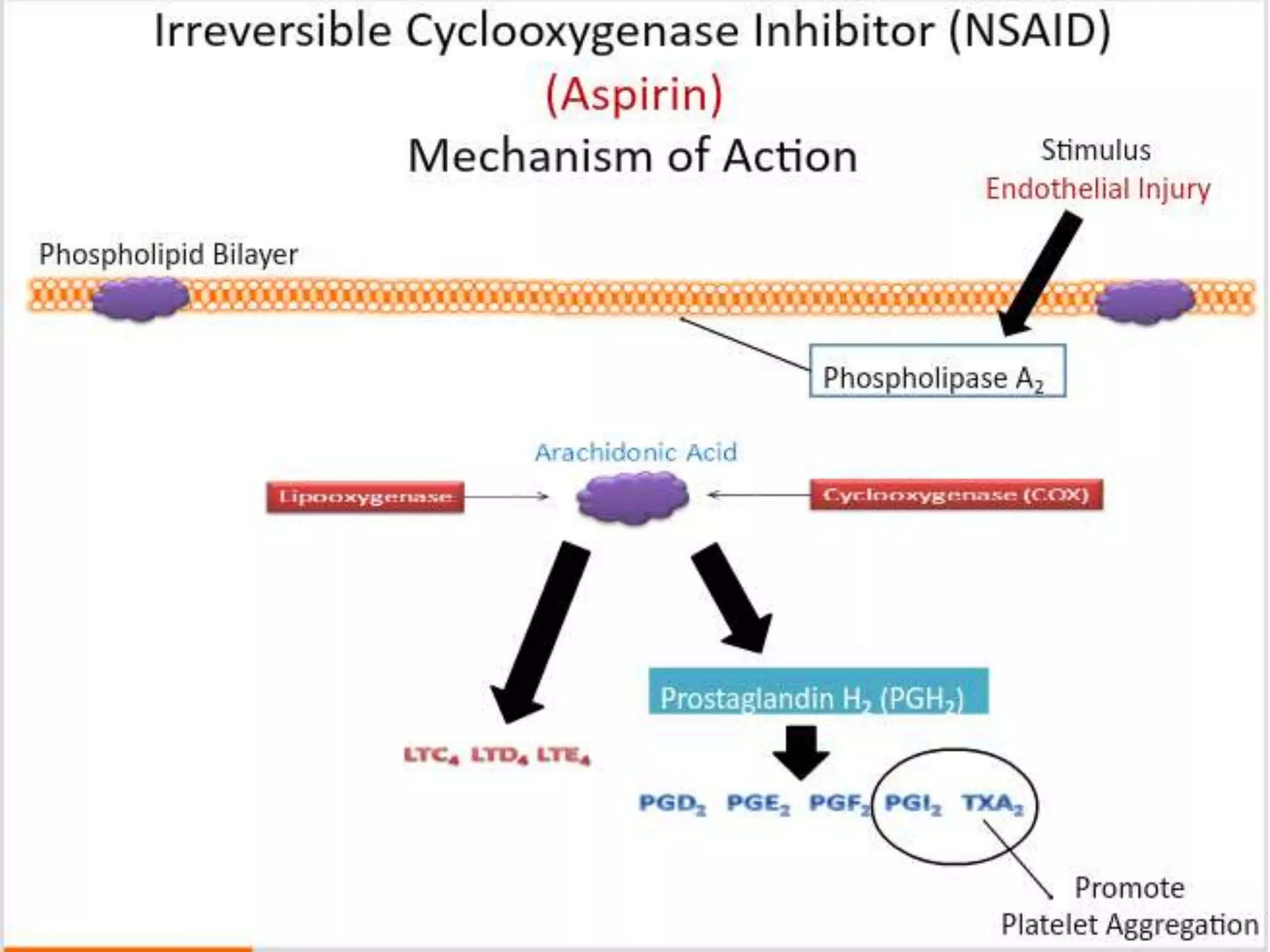
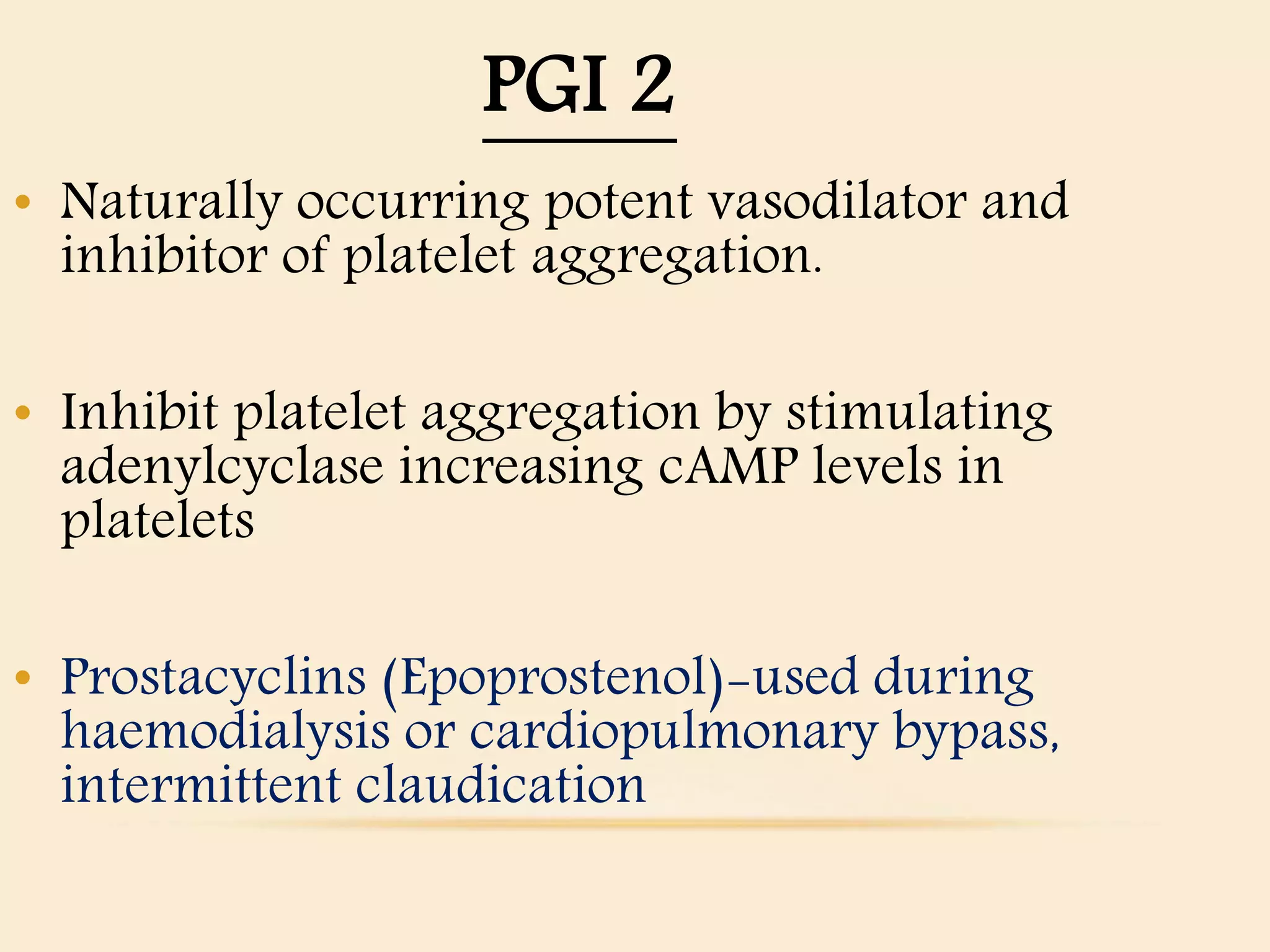
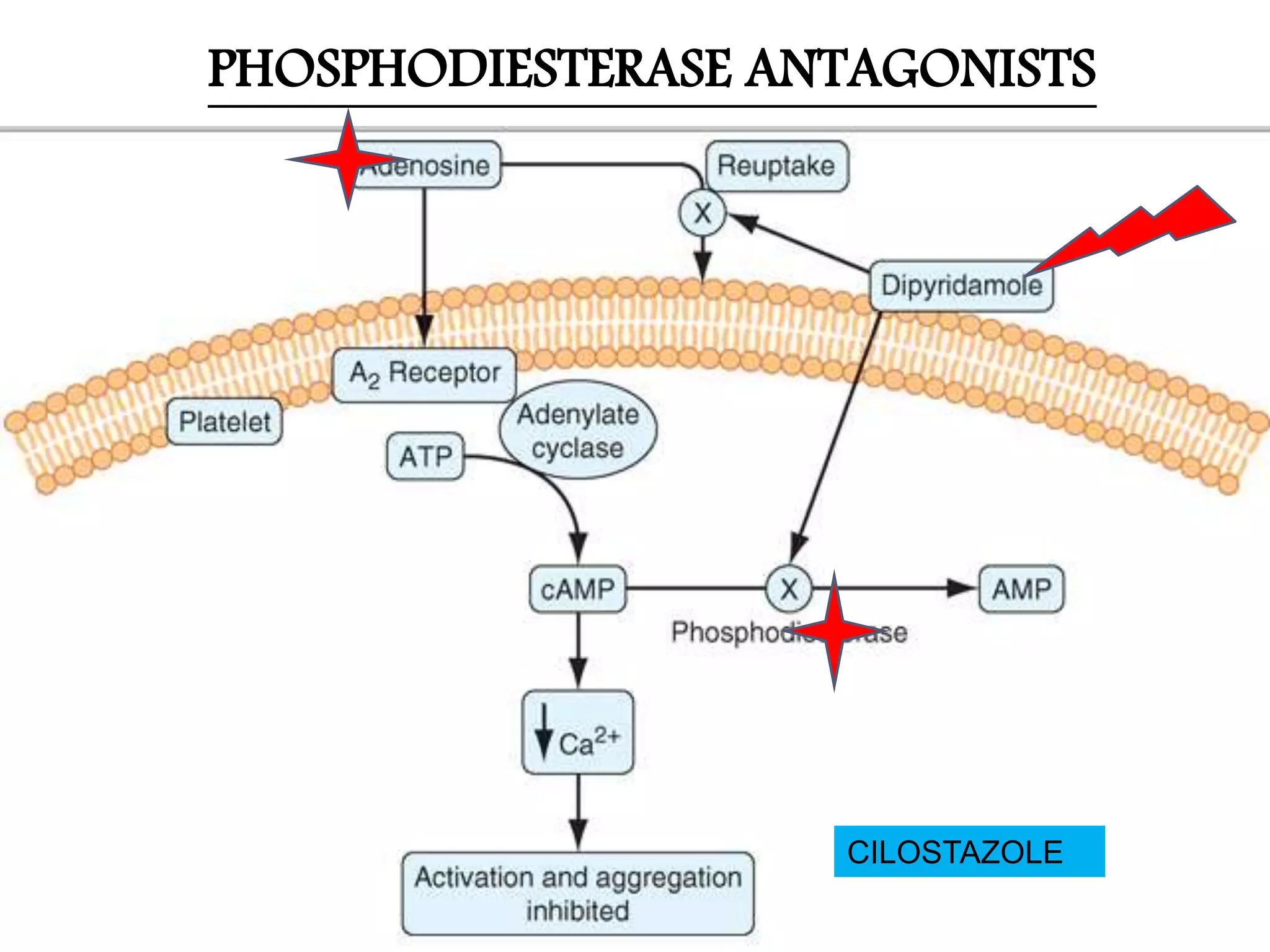
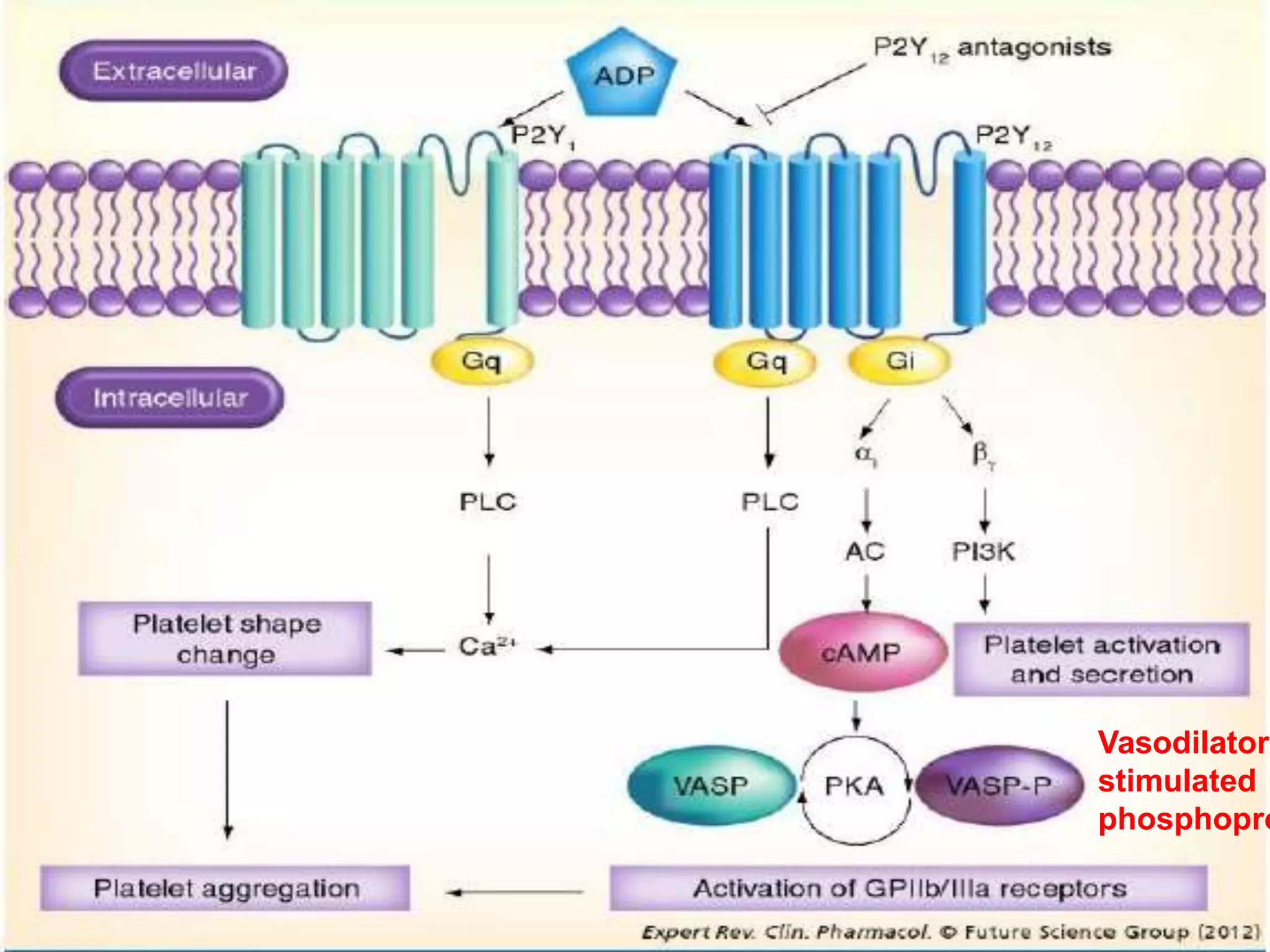
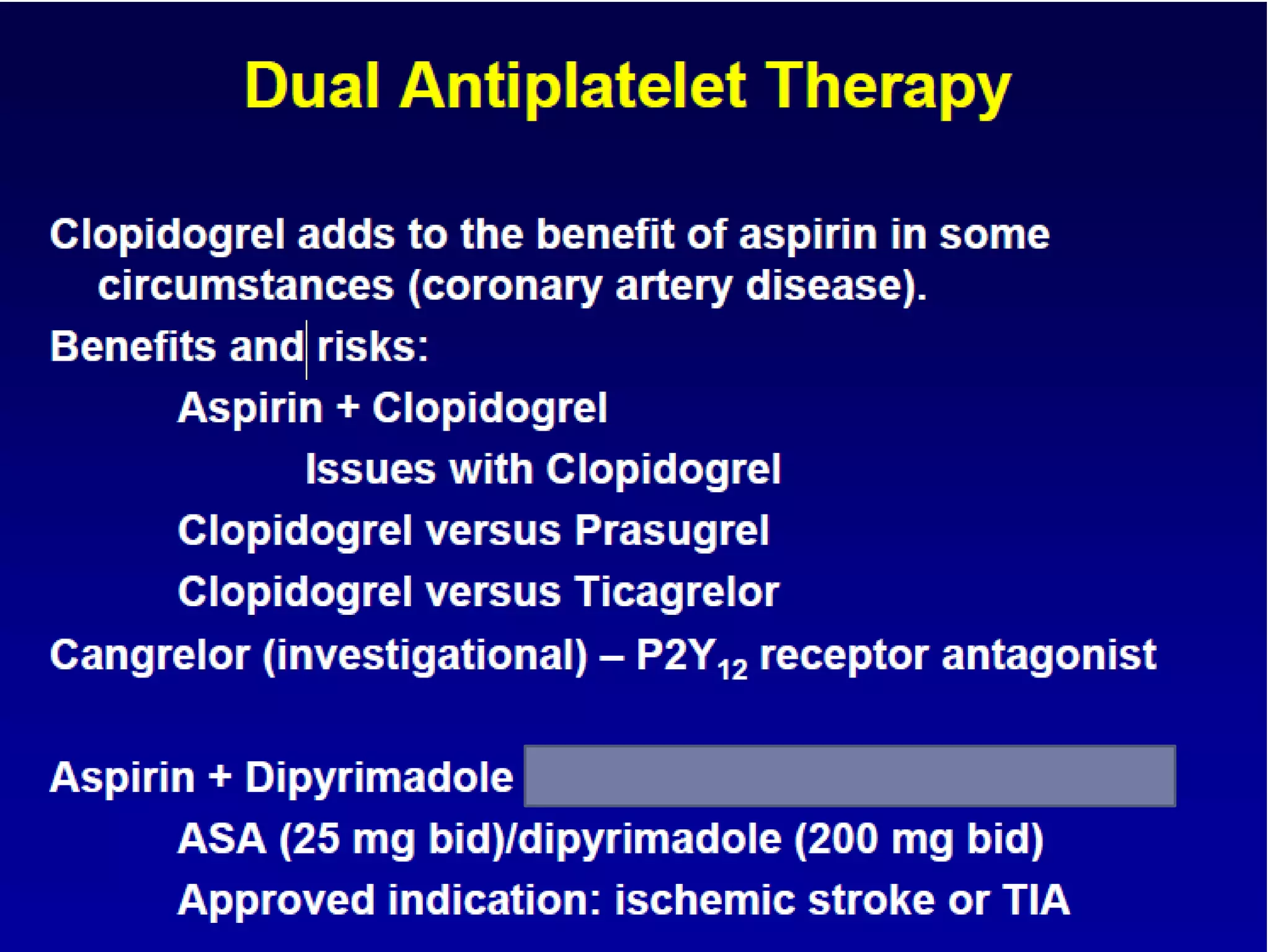
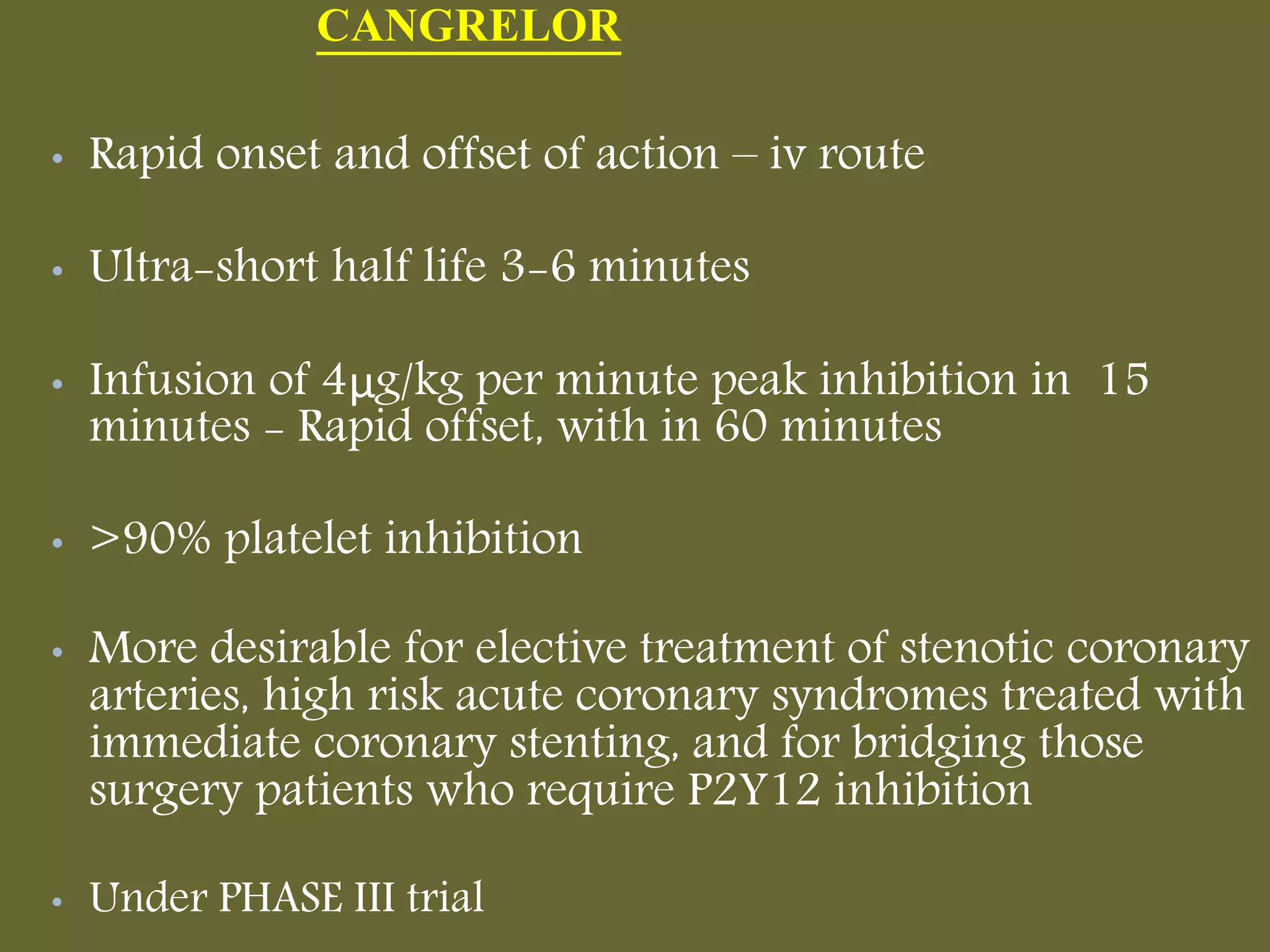
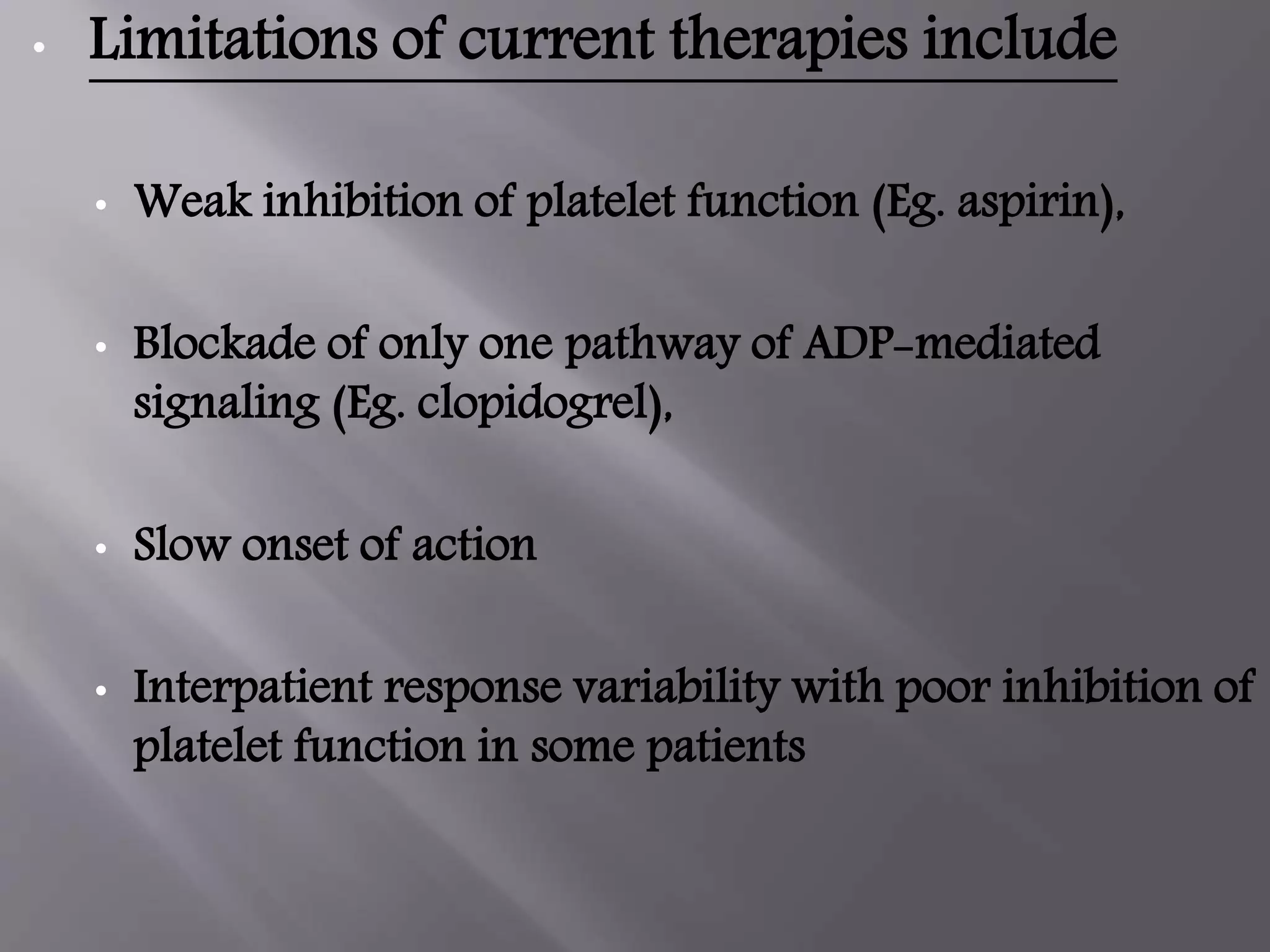
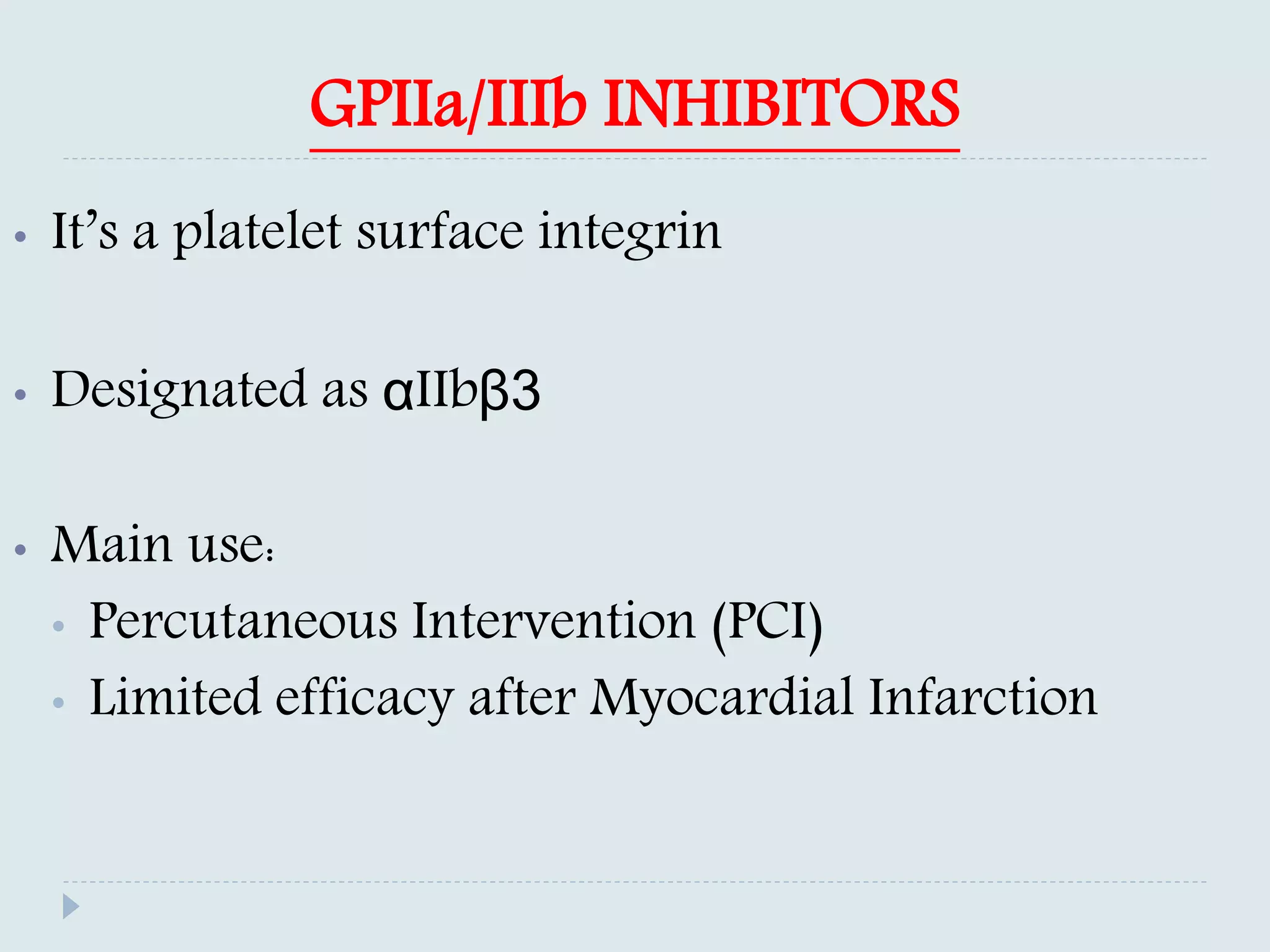
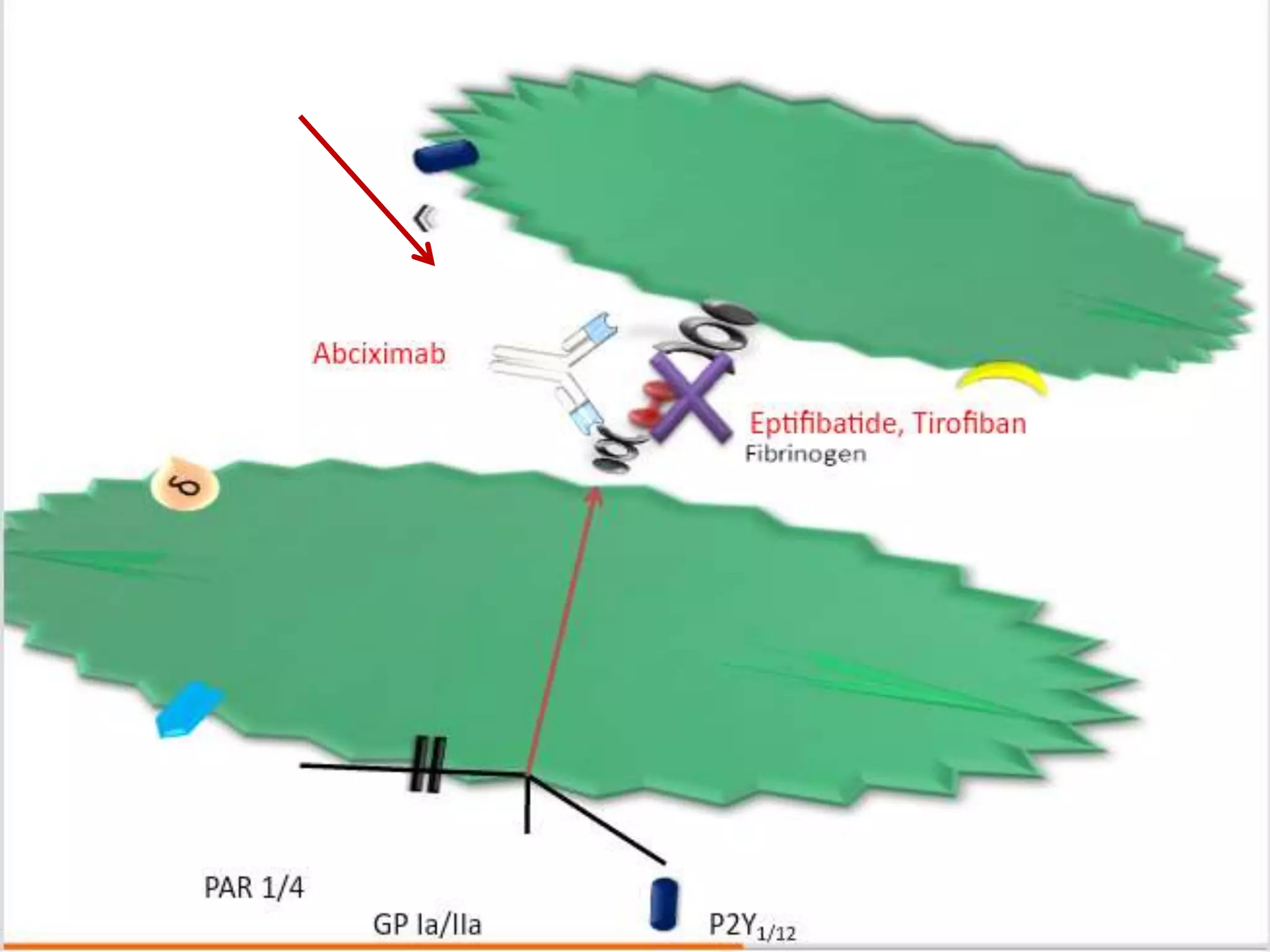
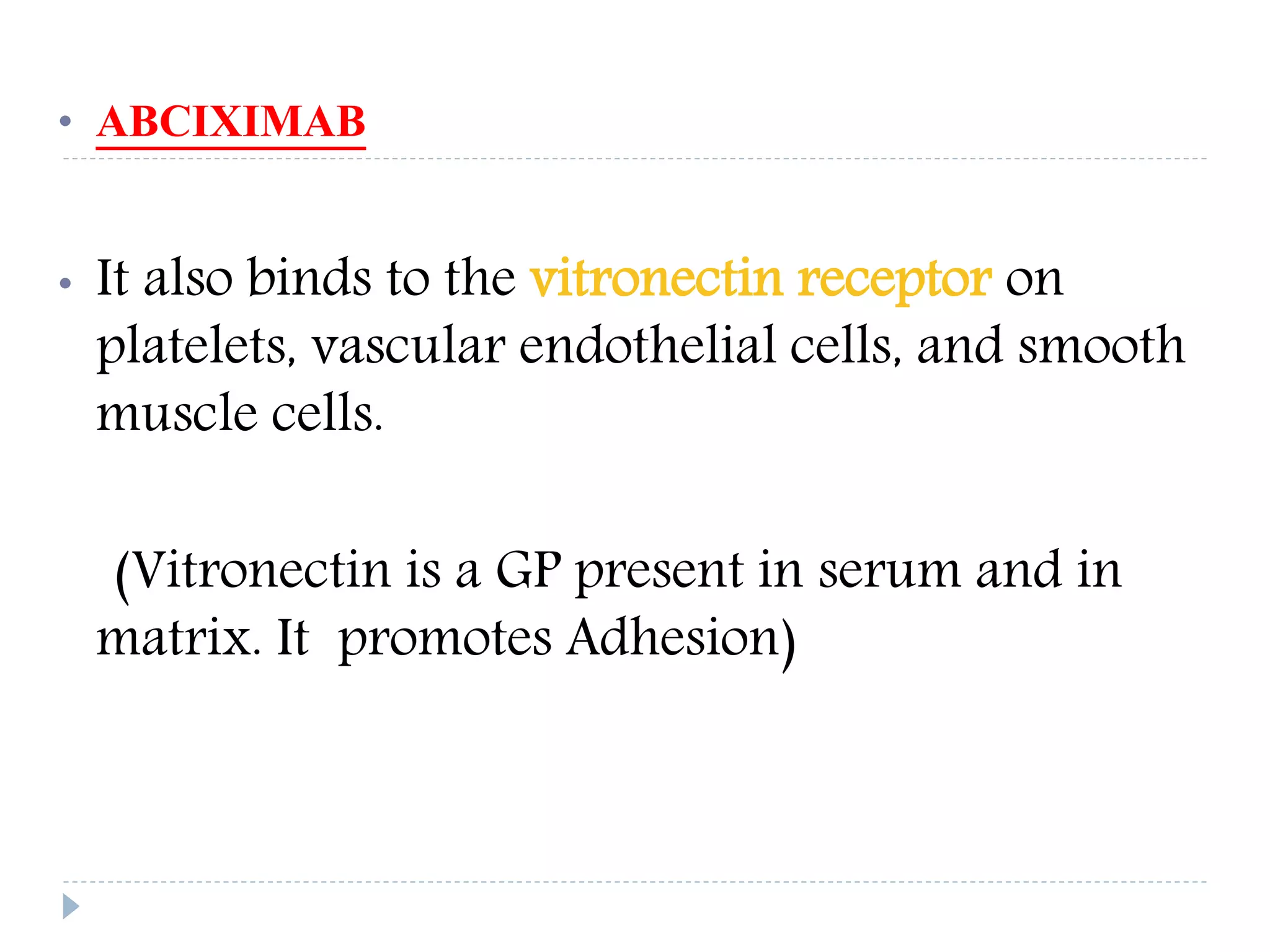
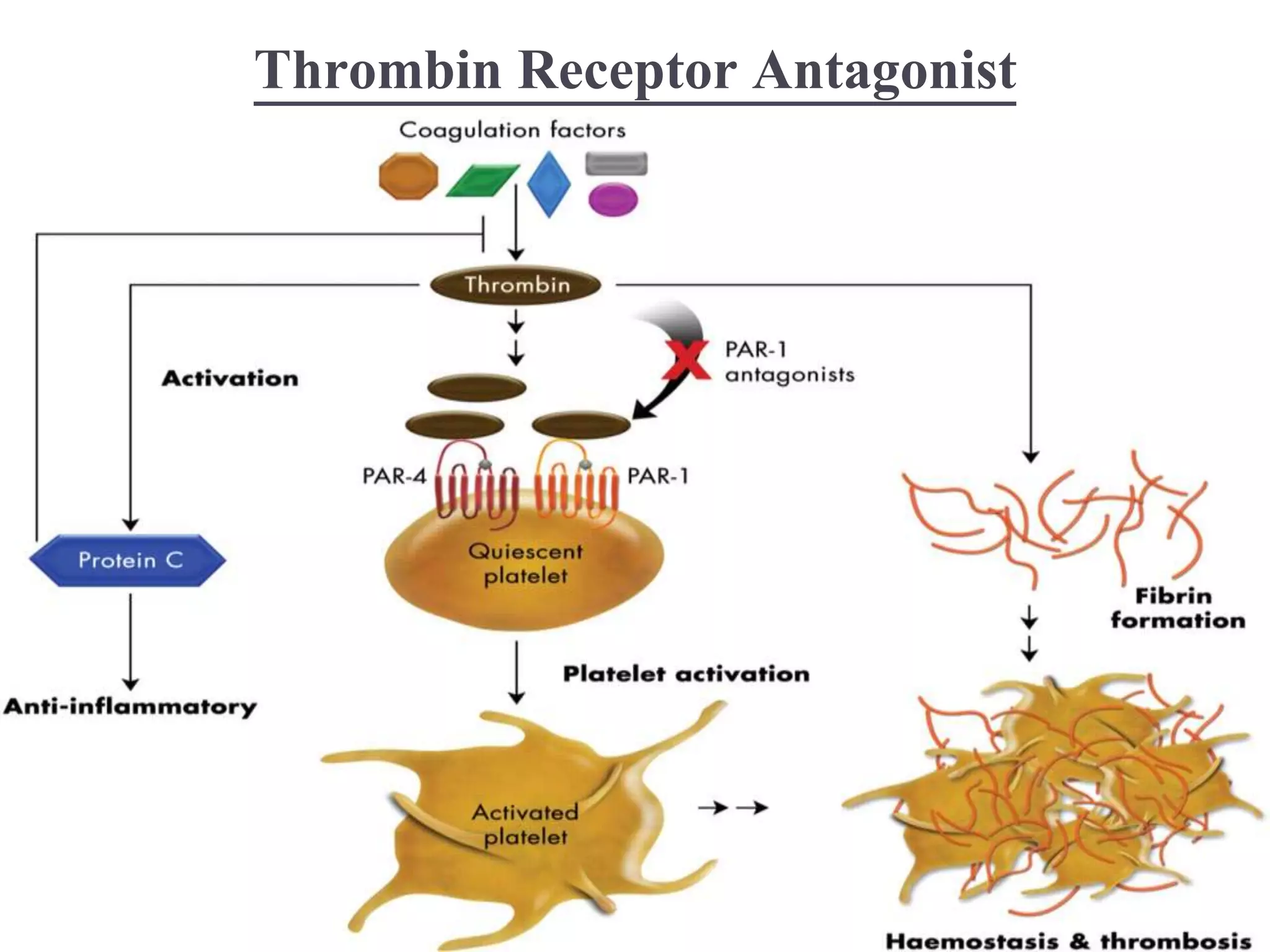
This document summarizes various antiplatelet drugs used to treat thrombotic diseases. It discusses the pathophysiology of thrombosis and hemostasis, focusing on the interplay between the vessel wall, coagulation proteins, and platelets. Older antiplatelet drugs such as aspirin, clopidogrel, and GP IIb/IIIa inhibitors are described along with newer agents like ticagrelor, elinogrel, and cangrelor that inhibit the P2Y12 receptor on platelets. Other drug classes discussed include thromboxane receptor antagonists, thrombin receptor antagonists, and GPVI receptor antagonists. The challenges of preventing thrombosis without increased bleeding risks are also noted.