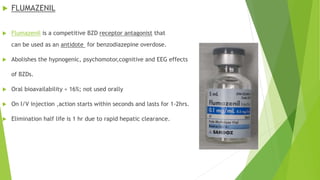
Diazepam poisoning occurs when excessive amounts are ingested. Symptoms develop rapidly and include impaired motor function, slurred speech, and nausea. Severe overdoses can cause prolonged coma, respiratory depression, and cardiac arrest. Treatment involves medical observation, supportive care, and intubation if needed to protect the airway. Flumazenil is an antidote but due to risks of withdrawal, it is rarely used and supportive care is usually sufficient.