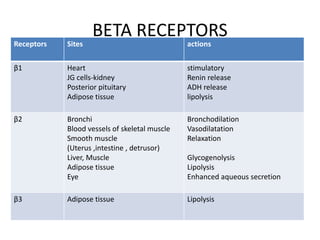
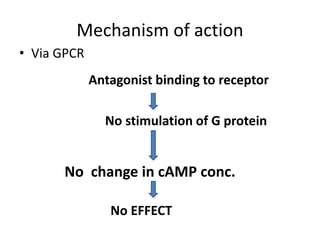
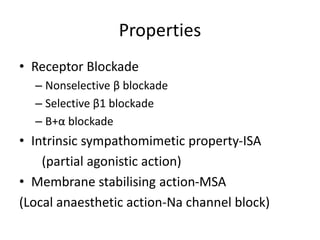
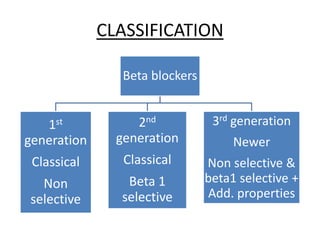
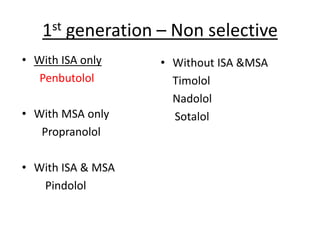
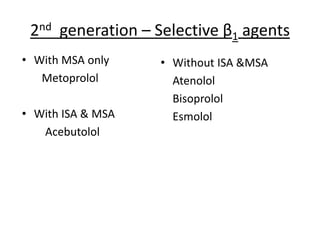
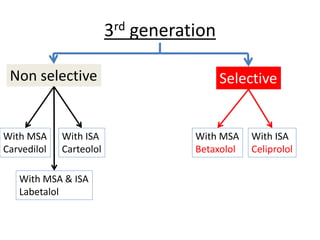
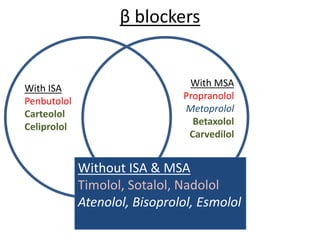
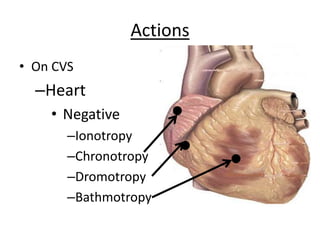
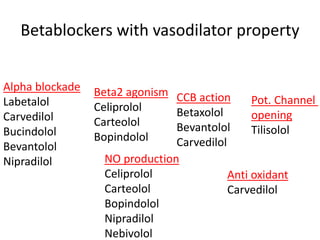
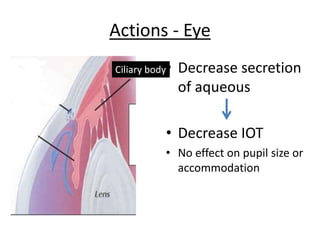
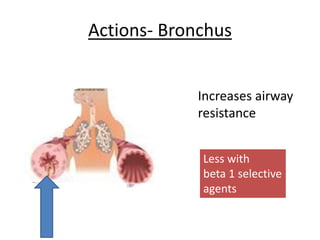
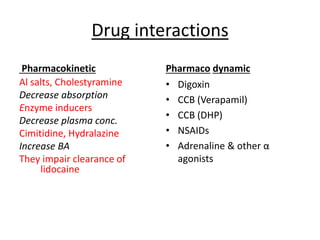
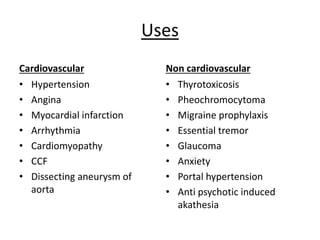
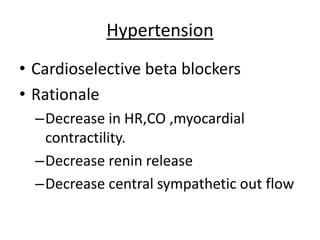
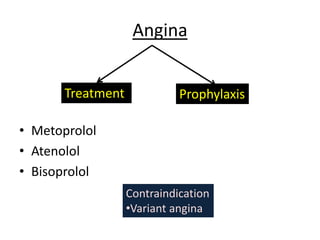
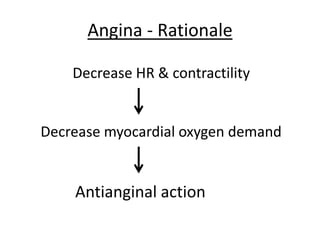
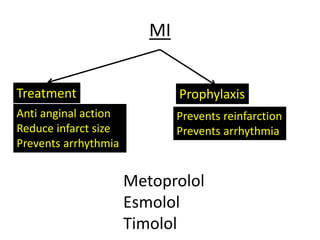
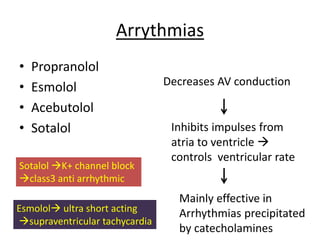
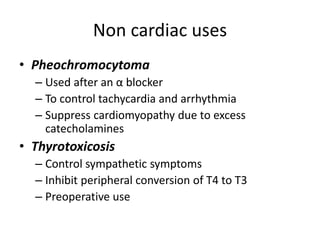
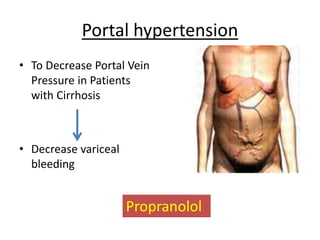
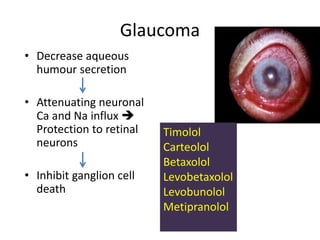
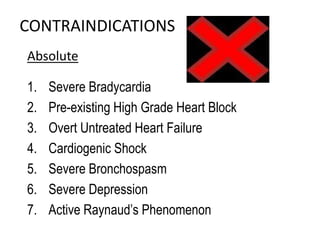
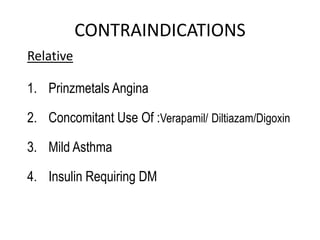
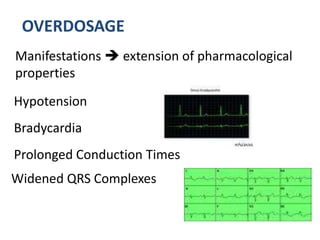
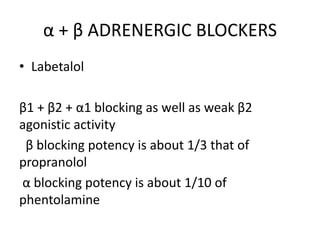
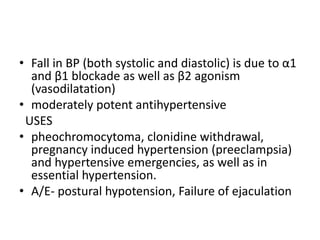
Beta blockers are medications that inhibit adrenergic responses mediated by beta receptors, affecting various physiological actions in the heart, blood vessels, and other tissues. They are classified into three generations based on selectivity and additional properties, with indications for use in cardiovascular and non-cardiovascular conditions such as hypertension, angina, and anxiety. Adverse effects may include bradycardia, respiratory issues, and metabolic alterations, with specific contraindications for certain populations.